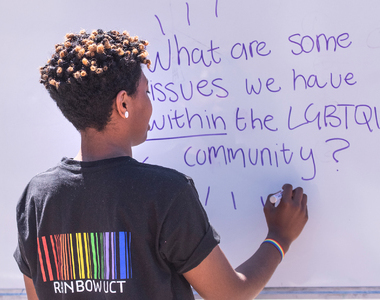
Integrate mental health support into HIV care
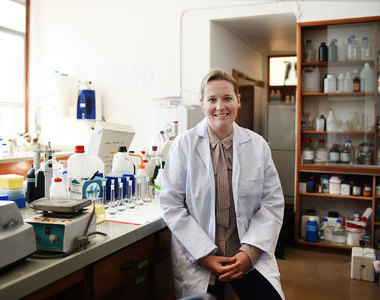
03 February 2026 | Story Ridovhona Mbulaheni. Photo Unsplash. Voice Cwenga Koyana. Read time 4 min.
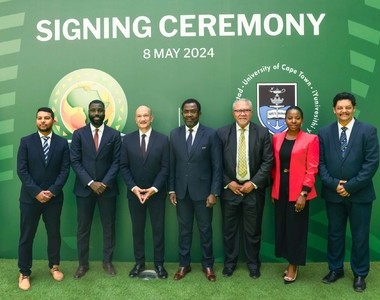
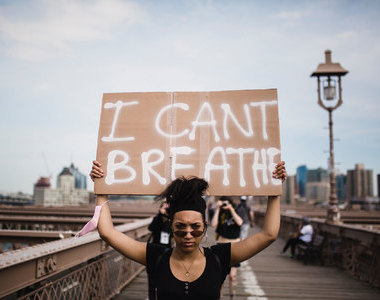
People living with HIV face an elevated risk of suicide due to compromised mental health, according to a new research study led by academics at the University of Cape Town (UCT), in partnership with colleagues at Linköping University in Sweden.
The stigma associated with an HIV diagnosis, fear of victimisation when disclosing HIV status and the gaping holes in South Africa’s primary healthcare system are just some of the reasons that make people living with HIV vulnerable to die by suicide. Therefore, the study highlights the importance of integrating mental health support into HIV care to assist people living with HIV as they navigate their diagnosis and the road ahead.
Published in the AIDS Care Journal, the study explores healthcare workers’ perspectives on the risks, barriers to care and prevention needs in primary healthcare settings. As part of the research, the team conducted interviews with 13 healthcare workers who work in three different primary healthcare clinics in Khayelitsha.
“Suicide disproportionately affects people living with HIV.”
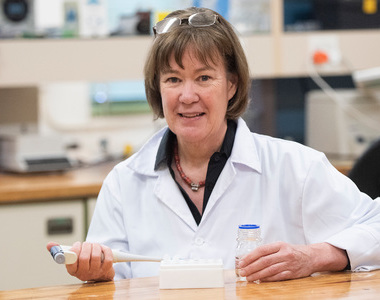
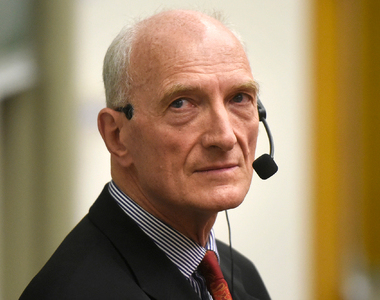
“Suicide disproportionately affects people living with HIV. The reasons for this elevated risk are complex and multifaceted. There isn’t one specific casual pathway that can explain why people with HIV are particularly vulnerable to die by suicide. Rather, people with HIV are confronted by a combination of situational stressors that compromise their mental health and increase their risk for suicide,” said Associate Professor Stephan Rabie, a chief research officer in UCT’s Department of Psychiatry and Mental Health and the study’s principal investigator.
And the elevated risk of mental illness and related suicide outcomes has far-reaching implications across the HIV continuum, Associate Professor Rabie said. This includes delays in treatment initiation, poor engagement with HIV care and a reduced life expectancy.
Contributing factors
He said past research revealed that individuals who die by suicide often visit a healthcare setting 12 months before their death. But in South Africa in particular, where the bulk of people living with HIV receive care in the public health sector, opportunities to screen for and prevent suicide, among those who seek care in community-based health facilities, remain underutilised.
“Our findings showed that among people living with HIV, suicidal ideation and behaviour are driven by a confluence of stressors, such as experiencing rejection after disclosing HIV statuses, and general social stressors like unemployment and financial deprivation,” he said.
Unlike high-income countries, where psychiatric disorders drive suicide cases, Rabie said, low-resourced settings like South Africa show that socio-economic challenges such as unemployment and food insecurity significantly contribute to suicidal behaviour.
Preventing suicide
Rabie said the research found that one of the main barriers to preventing suicide was the lack of routine screening for suicide and limited training in suicide risk assessment among primary healthcare workers.
“Providing opportunities for training in suicide risk assessment that are accessible and not burdensome to healthcare workers will be an important first step in addressing the syndemic of suicide in South Africa,” he said.
“This intervention will be pilot tested in primary healthcare facilities in the Cape Metro in 2026.”
The study also identified two additional strategies to improve suicide prevention among people living with HIV. These, he said, include integrating mental health care in HIV clinical settings and implementing brief interventions to support primary healthcare workers to address the multifaceted factors that influence suicide among people living with HIV – such as counselling programmes focussed on psychoeducation and suicide risk factors.
“These findings will inform the development of a brief intervention that introduces brief safety planning to reduce suicide risk and [provide] training in adaptive coping skills, to manage the stress that derives suicide ideation and behaviour. In partnership with the City of Cape Town and the Western Cape Department of Health and Wellness, this intervention will be pilot tested in primary healthcare facilities in the Cape Metro in 2026,” Rabie said.
This study was supported by the Fogarty International Centre and the National Institutes of Mental Health in the United State of America.
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.
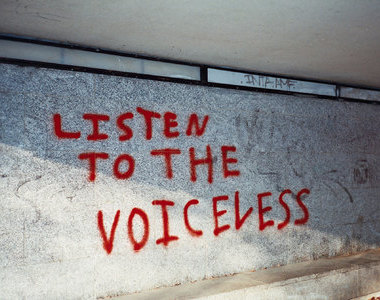
Listen to the news
The stories in this selection include an audio recording for your listening convenience.