Modelling a pandemic on scarce data and unknowns
24 July 2020 | Story Gesine Meyer-Rath, Sheetal Silal, Juliet Pulliam and Harry Moultrie. Photo Wikimedia Commons. Read time >10 min.
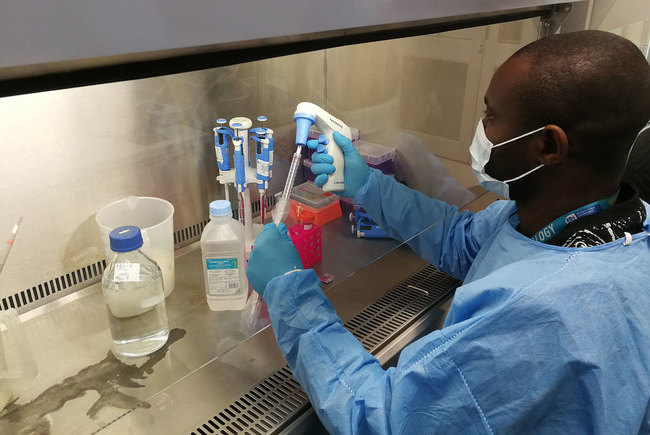
As a member of the South African Covid-19 Modelling team, University of Cape Town (UCT) academic Dr Sheetal Silal, a senior lecturer in the Department of Statistical Sciences, is using mathematical modelling to better understand the COVID-19 pandemic, sorting the known from the unknown, and the unknown from the unknowable, to produce estimates that may help government prevent a dangerous breaching of healthcare capacity and a dramatic increase in mortality.
A group of modellers recently put out a manifesto specifying "five ways to ensure that models serve society", with specific application to models hoping to serve societies' understanding of the Covid-19 pandemic. [1]
They summarise the uncertainty regarding almost all central aspects of how SARS-CoV-2 (the virus that causes Covid-19) behaves, including its prevalence, reproduction rate, the proportion of infected people who remain asymptomatic, the role of seasonality, whether cross immunity to the virus from other infections exists, and whether immunity to the virus itself persists – as well as the impact of any of the currently available non-pharmaceutical interventions such as physical distancing and mask wearing.
This uncertainty means that making decisions regarding anything from how seriously to take the virus to what to do to contain it, is based on shaky grounds; and yet, decisions have to be made by governments around the world.
In this situation, the manifesto implores us that “[m]odellers must not be permitted to project more certainty than their models deserve; and politicians must not be allowed to offload accountability to models of their choosing”.
Based on our collective experience of modelling Covid-19 for the South African government over the past four months, we concur.
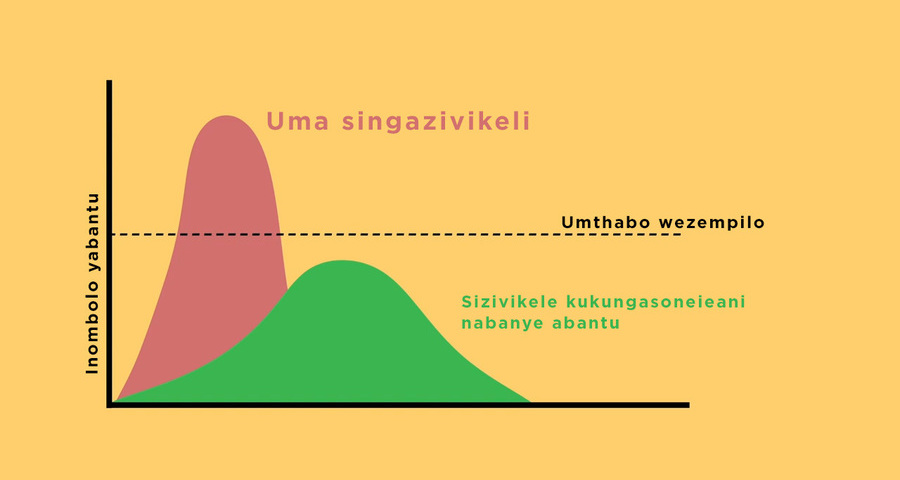
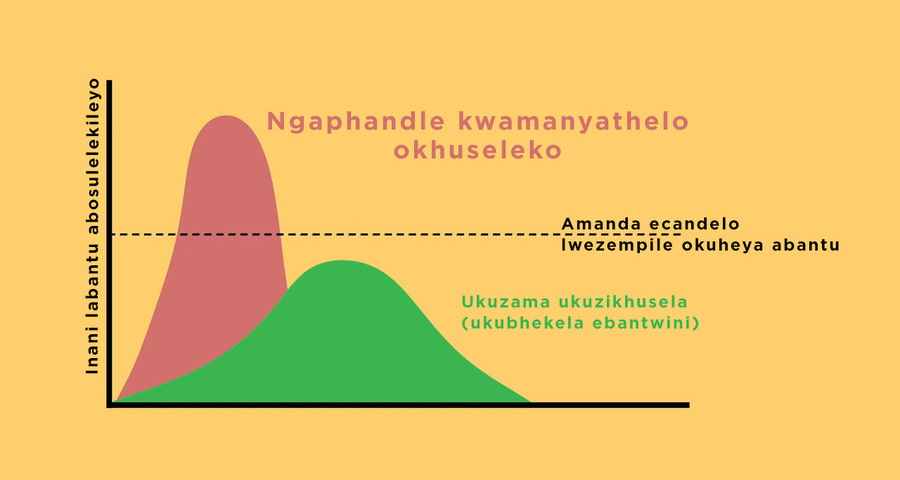
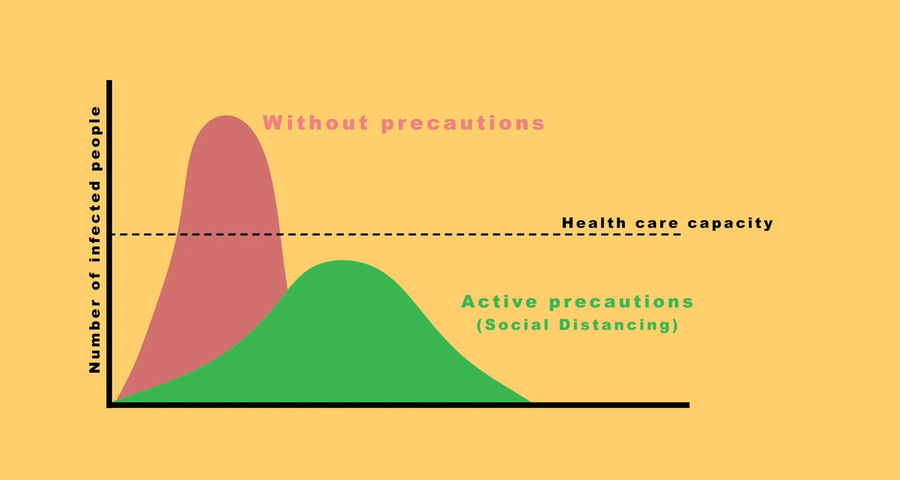
Sorting the known from the unknown, and the unknown from the unknowable, all while producing estimates that can help prevent a dangerous breaching of healthcare capacity with an ensuing dramatic increase in mortality, is what we understand to be our task.
The National Covid-19 Epi Model
Much has been written in the past weeks about the models used by government to make decisions regarding the management of the Covid-19 pandemic in South Africa.
Some of this was aimed at the National Covid-19 Epi Model (NCEM), of which we are the authors.
The National Covid-19 Epi Model is a stochastic compartmental transmission model designed to estimate the total and diagnosed number of Covid-19 cases at provincial and district level in South Africa.
The outputs of the model are used to inform resource requirements and predict where gaps could arise based on the available resources within the South African health system. The model follows a generalised Susceptible-Exposed-Infectious-Recovered (SEIR) structure accounting for disease severity (asymptomatic, mild, severe and critical cases) and the treatment pathway at outpatient level and into non-ICU and ICU care.
The model is being updated regularly as new data from South Africa and evidence from countries around the world become available. We do so to conscientiously fulfil the model’s main aim – to provide relevant, timely estimates of the number of Covid-19 cases, including severe cases needing hospitalisation, to allow the national and provincial departments of health to plan for the number of people needing care.
From the start, these projections have been used as inputs into a second model, the National Covid-19 Cost Model, which estimates the number of additional hospital beds, staff, and ventilators and oxygen volumes needed for inpatient care, as well as its costs – but also the likely number and costs of the PCR tests for SARS CoV-2, quarantine facilities, field hospitals, and staff at primary healthcare facilities.
All model updates find their way into the planning process immediately, after review through the consortium and relevant partners at the NDOH. We also endeavour to make the main outputs, scenarios and assumptions available to the public in the form of public releases available on the NICD website, although we have not been able to do this as frequently as we and the public would have liked, for no other reasons than the constraints on our time.
To construe this as us trying to hide something is incorrect; on the contrary, we have aimed at making all model outputs and code available for public scrutiny from the beginning.
What we got right – and what we got wrong
Another issue of public importance is the model’s degree of accuracy.
There remains considerable uncertainty regarding the likely trajectory of the Covid-19 epidemic in South Africa overall, and perhaps more so due to recent flattening of the growth in cases in the Western Cape.
We often hear the phrase that models are only as good as the data used to develop them.
This assertion is true, though models may be inaccurate for other reasons. Models may be mis-specified if they do not account for all the variables that are key to accurately estimating the desired outcome.
Additionally, the role of population behaviour in determining the trajectory and scale of the epidemic is more influential in Covid-19 due to the absence of a cure or vaccine.
We do not believe that one can precisely capture human emotion and behaviour in an equation, least of all in an unprecedented situation such as the current pandemic. To account for these unknowns, we present our estimates with uncertainty bands reflective of variation in the parameters driving the model and the model process itself.
While we acknowledge that model estimates may not always be accurate, there are aspects of the epidemic that we have predicted well, such as the overall national trend in the development of cases and deaths and, most importantly, the timing of capacity breaches. Our most recent published long-term projections (6 May) predicted 822 (prediction interval: 431–1 618) deaths nationally under the optimistic scenario, and 5 486 (2 849–9 869) deaths under the pessimistic scenario by 1 July.
Our short-term projections (12 June) for deaths on 1 July were 3 810 (1 880–7 270). The reported national Covid-19 deaths on the 1 July were 2 952 which is within the range of both the short- and long-term predictions.
There are instances, however, where the development of the pandemic has taken us by surprise.
Thankfully, although unexpectedly, confirmed Covid-19 deaths in the Western Cape have plateaued for the past four weeks, and hospital admissions for Covid-19 in the Western Cape appear to have peaked on 22 June.
While the decline in admissions and plateau in mortality are welcomed, the explanation remains unclear.
Did we over-estimate Covid-19 deaths in the Western Cape?
The brief answer is that we don’t know.
There are at least two possible explanations for the lower than projected Covid-19 deaths in the Western Cape.
Firstly, not everyone may be equally susceptible to Covid-19.
While this thesis has been promoted by other groups for a few months, the evidence remains scanty. There are indications that children may be less susceptible to SARS-CoV-2 (the virus that causes the Covid-19 disease) and that previous exposure to other coronaviruses could possibly provide T-cell derived immunity to SARS-CoV-2.
If either or both of these mechanisms is at work, then the proportion of the population susceptible to Covid-19 will be lower than that predicted in our models, resulting in lower Covid-19 mortality.
This would be good news; however, we do not yet have robust enough evidence regarding the presence and level of existing immunity to take this into account in more than a hypothetical scenario.
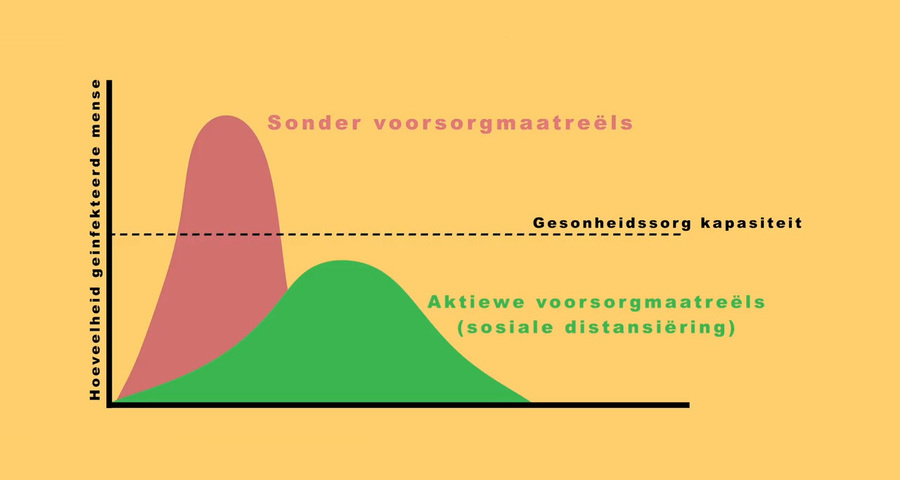
Secondly, public awareness of increasing deaths and the looming threat of overwhelmed healthcare facilities in the Western Cape, combined with communication campaigns, could have resulted in better adherence to NPIs (e.g. masks, hand washing and physical distancing) and in those most at risk for severe Covid-19 disease taking additional precautions to isolate themselves.
Since individual behaviour changes are unpredictable and difficult to model, these are not included in our models.
It is probable that the explanation is a combination of these factors. We simply don’t know yet, and it is too early to infer from the change of the Western Cape curve how the curves for the other provinces or the country overall will likely change.
The curious ‘flaw’ of regular updates
Models that incorporate and try to make sense of as much uncertainty as those estimating Covid-19 cases and associated resource use can only stay relevant and contribute to planning when they are updated as soon and as often as new evidence becomes available – be it in the shape of new local statistics or international evidence.
As a result, projections differ between individual public releases and internal updates, sometimes by quite a bit.
This is another "flaw" that has most recently been held against our model; we however maintain that it is our duty to update as often as we can, while taking care to communicate the reasons for each update in a transparent manner, and presenting results alongside potential factors that could change them in the future.
Among the elements that we have updated regularly is the reproductive number, both in terms of taking differences between increasingly smaller areas into account as soon as the growing case numbers allowed us to do so, and in terms of updating our assumptions about the adherence of the population to the restrictions.
In past updates, we have had to decrease our assumptions regarding the reproductive number across all provinces, based on analyses taking the lower than expected number of cases into account.
Possible reasons for this include, but are not limited to, better adherence to restrictions than we had initially assumed, and heterogeneity in susceptibility or mixing patterns.
As a result, the projected peaks in each province have moved further apart, which allows scarce in-patient resources to go further, resulting potentially in fewer deaths from breaching the current capacity of ICU and other hospital beds and the staff who work there.
This is good news with regards to the combined resources needed for the Covid-19 response as well as the required budget.
Outlook on new updates
We will continue to update our numbers, and so will the teams planning, budgeting for, and ordering resources to deal with this pandemic in each province.
Amongst the next planned updates are the incorporation of mortality resulting from a potential breach of the bed capacity; the update of the inpatient care pathways in the model to incorporate non-ICU care options such as oxygen delivery via high-flow nasal cannulae; and new treatment options such as dexamethasone, remdesivir and interleukin-6 inhibitors if they are incorporated into local guidelines, as well as the additional capacity that the planned field hospitals might provide.
As mentioned, we are planning to make the model code public for additional scrutiny.
With these updates, we continue to strive towards making our models as useful as possible, while bearing in mind the assertion of the above mentioned manifesto that "[m]athematical models are a great way to explore questions. They are also a dangerous way to assert answers. Asking models for certainty or consensus is more a sign of the difficulties in making controversial decisions than it is a solution".
– Gesine Meyer-Rath, Sheetal Silal, Juliet Pulliam and Harry Moultrie from the South African Covid-19 Modelling Consortium
[i]Saltelli A, Bammer G, Bruno I, et al. Five ways to ensure that models serve society: a manifesto. Nature 2020; 582(7813): 482-4.
Coronavirus Disease 2019 updates
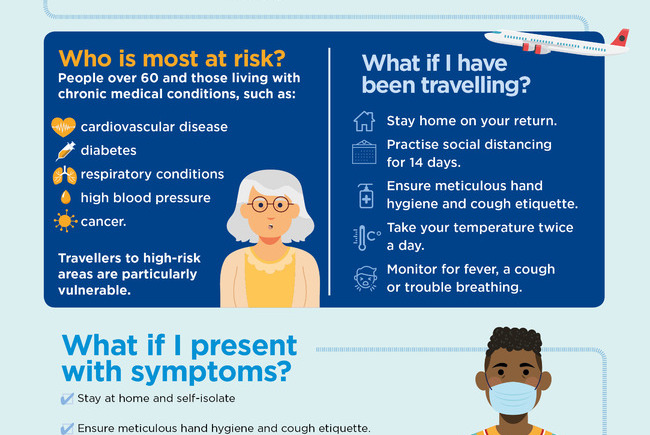
COVID-19 is a global pandemic that caused President Cyril Ramaphosa to declare a national disaster in South Africa on 15 March and implement a national lockdown from 26 March.
UCT is taking the threat of infection in our university community extremely seriously, and this page will be updated regularly with the latest COVID-19 information.
Daily updates
Campus communications
Resources
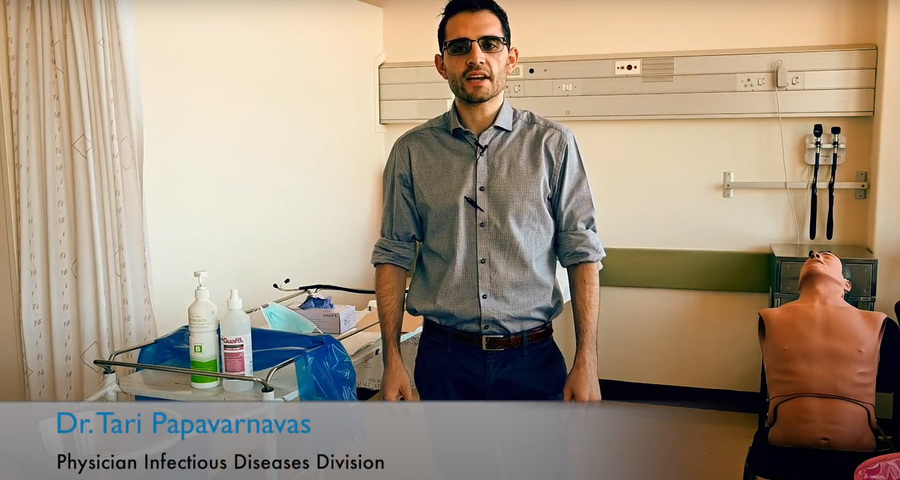
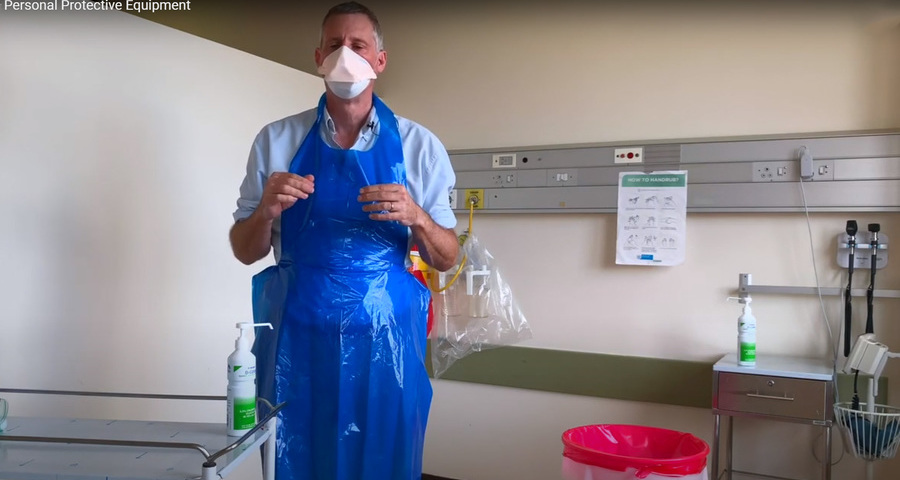
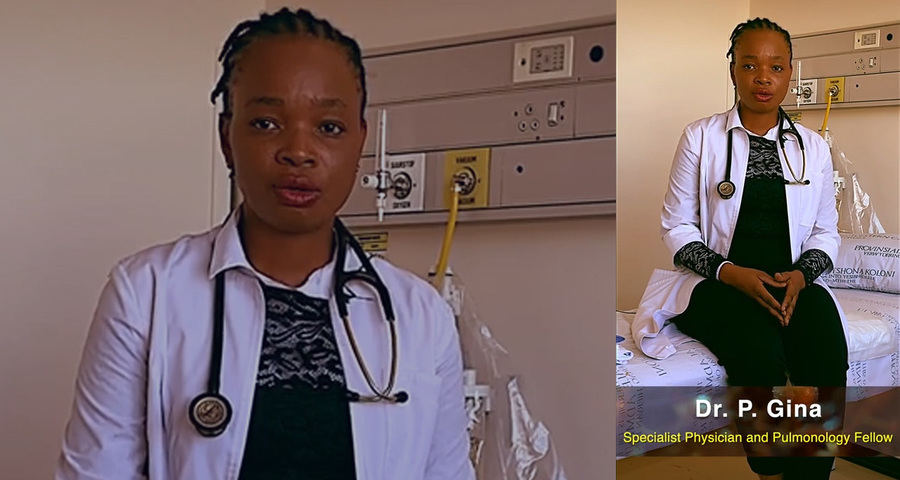
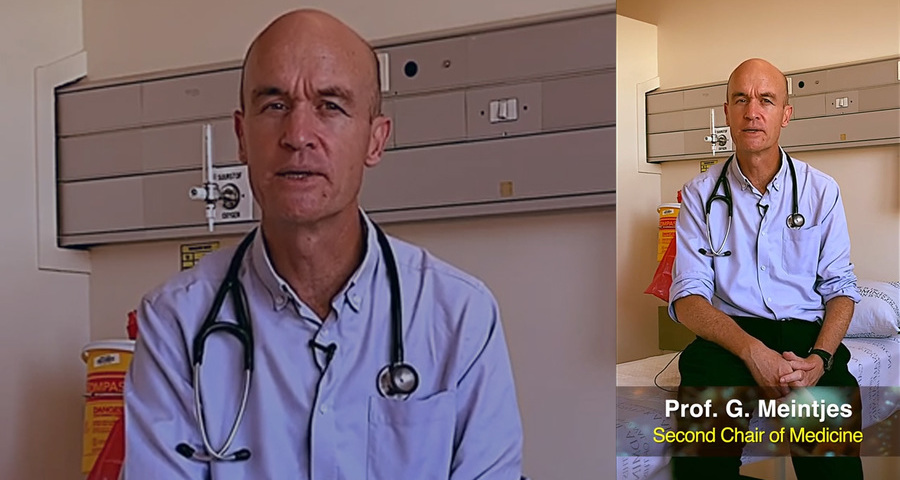
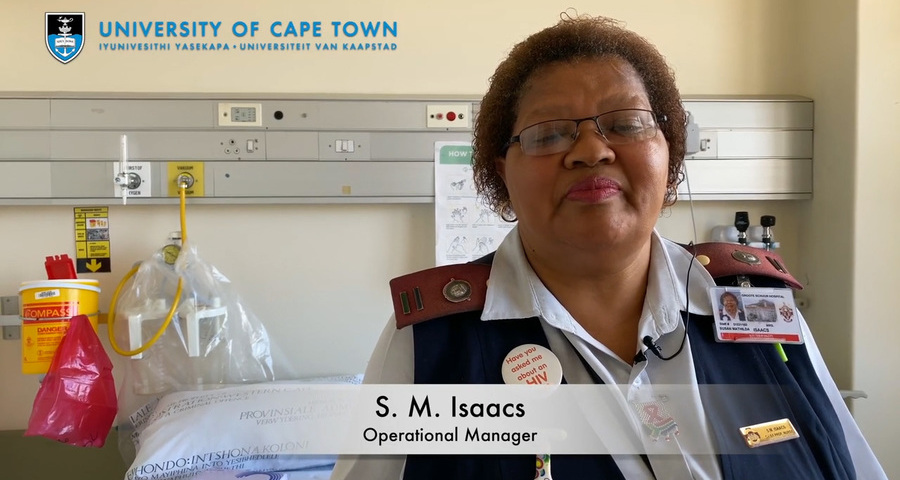
Video messages from the Department of Medicine
Getting credible, evidence-based, accessible information and recommendations relating to COVID-19
The Department of Medicine at the University of Cape Town and Groote Schuur Hospital, are producing educational video material for use on digital platforms and in multiple languages. The information contained in these videos is authenticated and endorsed by the team of experts based in the Department of Medicine. Many of the recommendations are based on current best evidence and are aligned to provincial, national and international guidelines. For more information on UCT’s Department of Medicine, please visit the website.
To watch more videos like these, visit the Department of Medicine’s YouTube channel.
Useful information from UCT
External resources
News and opinions

As the COVID-19 crisis drags on and evolves, civil society groups are responding to growing and diversifying needs – just when access to resources is becoming more insecure, writes UCT’s Prof Ralph Hamann.
03 Jul 2020 - 6 min read Republished
The Covid-19 crisis has reinforced the global consequences of fragmented, inadequate and inequitable healthcare systems and the damage caused by hesitant and poorly communicated responses.
24 Jun 2020 - >10 min read Opinion
Our scientists must not practise in isolation, but be encouraged to be creative and increase our knowledge of the needs of developing economies, write Professor Mamokgethi Phakeng, vice-chancellor of UCT, and Professor Thokozani Majozi from the University of the Witwatersrand.
09 Jun 2020 - 6 min read Republished
South Africa has been recognised globally for its success in flattening the curve, which came as a result of President Ramaphosa responding quickly to the crisis, writes Prof Alan Hirsch.
28 Apr 2020 - 6 min read RepublishedStatements and media releases
Media releases
Read more
Statements from Government
In an email to the UCT community, Vice-Chancellor Professor Mamokgethi Phakeng said:
“COVID-19, caused by the virus SARS-CoV-2, is a rapidly changing epidemic. [...] Information [...] will be updated as and when new information becomes available.”
We are continuing to monitor the situation and we will be updating the UCT community regularly – as and when there are further updates. If you are concerned or need more information, students can contact the Student Wellness Service on 021 650 5620 or 021 650 1271 (after hours), while staff can contact 021 650 5685.