Conflict leaves children traumatised, anxious – for life
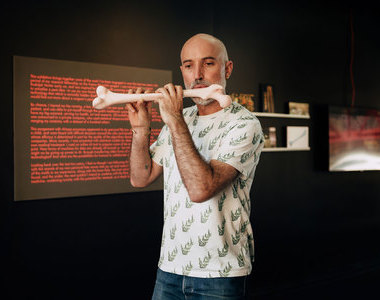
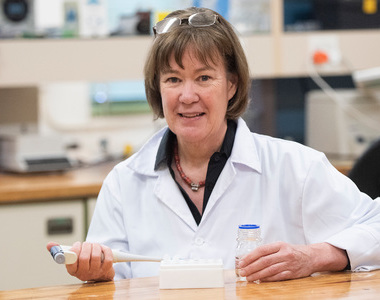
26 August 2019 | Story Helen Swingler. Photo Brenton Geach. Read time 7 min.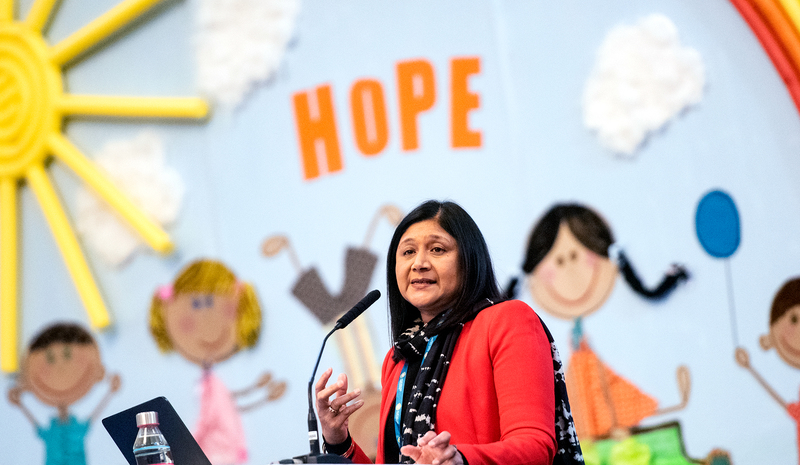
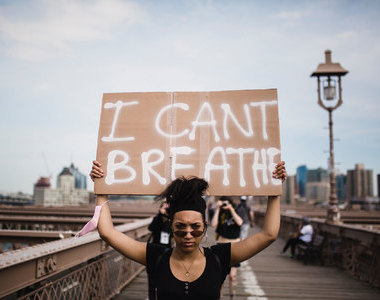
In Africa 14.5% of children under the age of 16 are suffering from the effects of violence – both collective and interpersonal violence – resulting in long-term trauma. In the Western Cape the prevalence is 17%, with post-traumatic stress disorder (PTSD) affecting 8% of under-16s and generalised anxiety disorder affecting 11%.
Trauma as a result of violence and adverse experiences in childhood is linked to a wide range of outcomes such as addiction, chronic physical conditions, depression and anxiety, self-harming behaviours and other psychiatric disorders.
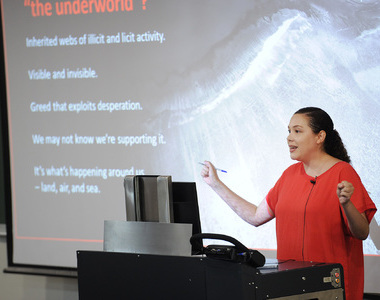
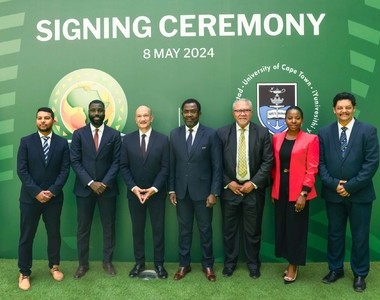
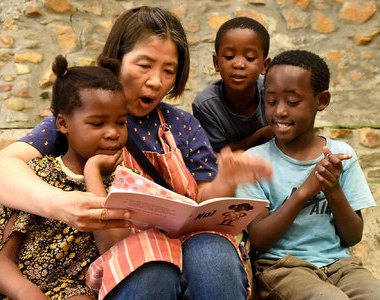
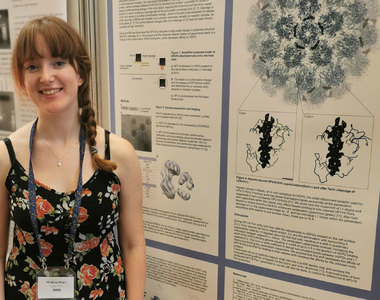
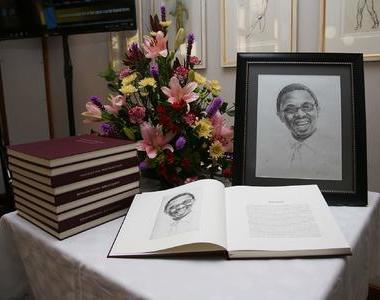
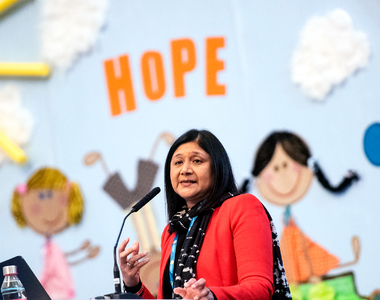
It’s critical to intervene early in these cases of trauma in children, said the University of Cape Town’s (UCT) Professor Shanaaz Mathews in her keynote address at The African Regional Child Trauma Conference 2019, which took place in the city from 18 to 21 August.
She continued: “This is essential to preventing injury and premature death, and lasting neurological and psychological damage in children.”
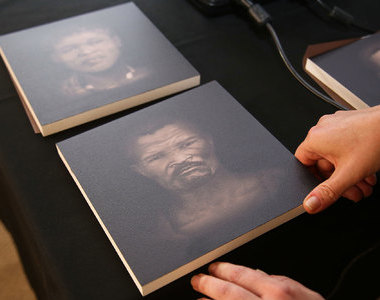
Mathews is the director of UCT’s Children’s Institute which was championing one of the main “streams” at the conference, highlighted under the banner: “The many faces of intergenerational trauma in Africa”.
Violence has characterised much of Africa’s documented history, she said, and although many historic accounts have focused on collective violence they have failed to highlight the various forms of pervasive interpersonal violence throughout the region.
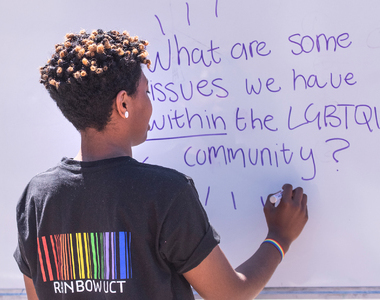
Intersecting forms of violence
Interpersonal violence, such as intimate partner violence, child abuse and neglect, are endemic across the continent, Mathews noted. But in zones of high conflict, intersecting forms of violence – interpersonal violence and collective violence – co-occur, resulting in both immediate and long-term trauma.
In the African context, she said, maltreatment of children is driven by a web of interrelated factors including extreme poverty, high levels of HIV, sociocultural variations in family structures and societal norms and values.
“Interpersonal violence, such as intimate partner violence, child abuse and neglect, are endemic across the continent.”
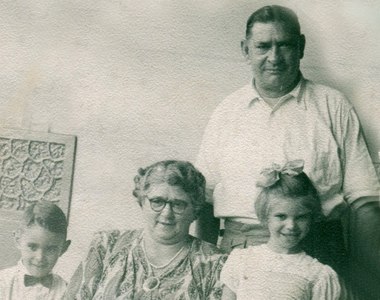
The most significant risk factors are maternal mental health problems, disruption of families, family structure, exposure to stressful events, maternal age and poverty-related issues. It is also important to understand the differences between transgenerational and intergenerational trauma, Mathews said.
“Transgenerational trauma is considered as the impact of violence being passed through generations, with the effects being evident without exposure to violence. With intergenerational trauma ... the experience or exposure to violence has occurred across generations of a family, with intergenerational effects.”
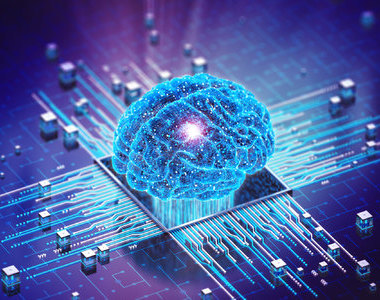
Early experiences of trauma can have lifelong effects on children, even marking them genetically.
“Experiences during a child’s development can rearrange the epigenetic markers that govern gene expression,” explained Mathews.
“Epigenomes are affected by both positive and negative experiences. Early experience of or exposure to violence causes epigenetic adaptations that influence how genes shape future health and resilience. Environmental influences can also affect how genes are expressed.”
Transgenerational trauma
She cited the example of the transgenerational impact of trauma and PTSD from Rwanda and the effect the Tutsi genocide had on children of women who were pregnant at the time of the genocide.
“In 2011, 16 years after the genocide, more than 20% of the Rwandan population met criteria for PTSD,” she said.
“In this study, mothers exposed to genocide and their children had significantly higher levels of PTSD and depression than a control group. Mothers and children exposed to trauma had a lower cortisol level than non-exposed mothers and their children – and lower cortisol levels were found to be related to PTSD.”
The danger for children exposed to prolonged neglect and abuse (toxic stress) can result in biological responses and damage the architecture of the developing brain. This increases the likelihood of significant mental health problems during childhood, or later in life, and importantly, impairs school readiness, academic success and both mental and physical health.
“Young children who experience recurrent abuse or chronic neglect, domestic violence or parental mental health [problems] or substance abuse are particularly vulnerable to toxic stress.”
In South Africa, polyvictimisation is common, where children are not safe at home, at school, in the community, in the company of their peers or in their intimate relationships with others.
“Victims can become trapped in a cycle of violence. With girls this increases the risk of revictimisation as adults…”
“Victims can become trapped in a cycle of violence,” Mathews noted.
“With girls this increases the risk of revictimisation as adults and heightens risks for internalising their experiences, causing depression, suicide and anxiety disorders.
“With boys, we see a cycle of perpetuating violence; increased chances of being violent in adolescence and adulthood and reduced ability to form attachments.”
The situation can be aggravated by patriarchal family structures, violence normalised as a means of discipline and to enforce gender norms. This leads to the normalisation of violence and the perpetration of intimate partner violence and violence against children.
Global picture
The global picture is sobering. In 2016 one in six children, or 357 million children, were living in conflict zones: 6% of those children in the Americas, 21% in Africa, 7% in Europe, 14% in Asia and 39% in the Middle East.
Violent conflict also destroys young lives in other ways.
“Children are recruited or forced to join armed forces as child soldiers, rape is systematically used as a weapon and young girls are often abducted and kept captive – with long-term physical and mental health consequences.”
“Caregivers’ own trauma must be recognised and managed for the child to get the necessary support.”
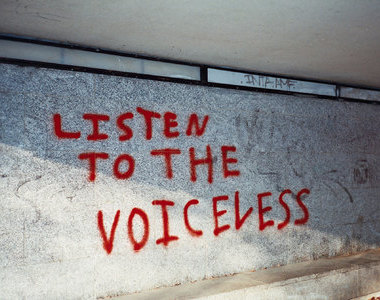
These outcomes in Africa are challenging. A shortage of health professionals and low capacity among non-specialist health workers to provide adequate care means that most children don’t get any treatment.
In South Africa, the regional economic powerhouse, there are 0.02 psychiatrists and 0.32 psychologists per 100 000 people working in the public health sector. Task-sharing or task-shifting has been proposed as a strategy to manage this shortfall.
In her recommendations, Mathews said society needs to address child trauma urgently to reduce its dire intergenerational legacy.
“Intergenerational trauma needs to be considered in therapeutic responses and caregivers’ own trauma must be recognised and managed for the child to get the necessary support.
“Complex forms of trauma need to be recognised and therapeutic approaches tailored to address the intergenerational complex nature of trauma in South African and other parts of Africa.”
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.
Listen to the news
The stories in this selection include an audio recording for your listening convenience.