COVID-19: Why critically ill patients in Africa are taking a bigger hit
24 May 2021 | Story Bruce M Biccard. Photo Paul Kagame. Read time 6 min.
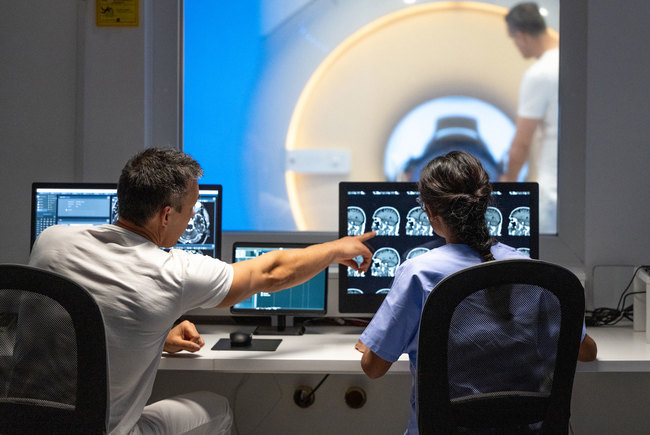
There have been insufficient data for African patients with COVID-19 who are critically ill. Therefore, the African COVID-19 Critical Care Outcomes Study, led by the University of Cape Town's Professor Bruce Biccard, has determined which resources, comorbidities, and critical care interventions are associated with mortality in this patient population.
In March 2020, those of us living on the African continent were terrified about what would happen. We had watched Wuhan and then Italy get overrun by COVID-19. These were environments far more resourced than Africa .
We knew that we had a limited healthcare workforce. And we have estimated that there was about one critical care bed per 100 000 population on the continent. The average across Europe was over 11 per 100 000 population.
What scared us even more was a lack of information about how to manage critically ill COVID-19 patients in resource limited environments. Steps were immediately taken to fill this void. The African Perioperative Research Group, an African research network, rapidly pivoted to conduct a continental study to determine resource, clinical factors and therapies associated with mortality or survival in critically ill patients.
The interim analysis was disseminated in a preprint last year to help healthcare providers. Now the full study of over 3000 critical care COVID-19 patients from 64 hospitals in 10 African countries has just been published.
The picture it paints is bleak. It shows that there have been excess deaths following COVID-19 critical care admission in Africa compared with the global average. And that the mortality of critically ill COVID-19 patients in Africa exceeded that of any other region in the world.
The bad news doesn’t end there. For every two COVID-19 patients referred for critical care treatment, only one was admitted to a high or intensive care unit. These patients in Africa have an excess mortality of between 11 and 23 extra deaths per 100 critical care admissions in Africa when compared to the global average. The mortality in Africa is 48.2%.
We suspect that these grim data probably provide an optimistic estimate of critical care outcomes on the continent. It is likely that the participating sites were relatively more resourced than other non-participating critical care units in Africa. Unfortunately, these data confirmed our fears when we set out on this project. Saving lives of critically ill COVID-19 patients in Africa is difficult for various reasons.
The grim reality
Our results show that even simple monitoring of patients was not universally available. One in ten hospitals could not provide pulse oximetry to measure arterial blood saturation to all critical care patients. Arterial desaturation is an important sign of a failure to adequately manage a severe respiratory disease such as COVID-19.
Pulse oximetry would be considered a basic requirement in critical care, and inadequate monitoring results in a delay to respond to deterioration. A delay in response is associated with mortality.
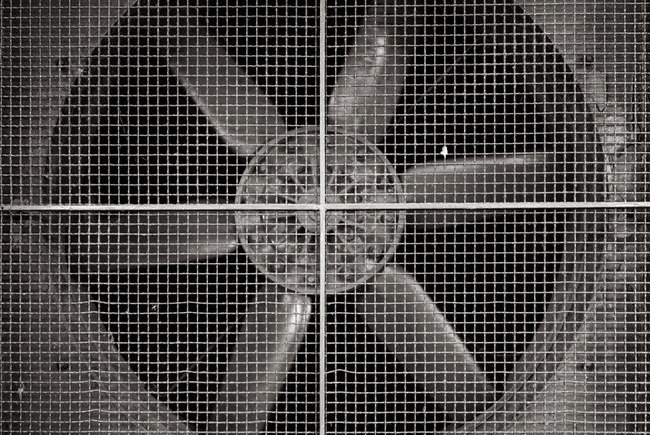
Secondly, there was insufficient equipment to provide advanced care at the participating sites. As a result, the ability to provide interventions (such as dialysis and proning (placing patients on their tummies)) was estimated to be delivered between seven and 14 times fewer than what would be expected for these patients based on the severity of their illness.
A commentary on our study also suggested caution when counting available equipment in Africa. It is well documented across Africa that a substantial amount of equipment doesn’t work. This is often because it has been donated and is not appropriate for the environment. There are also often no service contracts to maintain it.
The reality about scarce resources is that once a patient in the critical care unit is being given a particular therapy, such as dialysis, it is then unavailable to the other patients while in use.
These factors certainly would result in excess mortality.
Besides known risk factors for mortality in severe COVID-19 infection, our study also showed that HIV/AIDS was associated with an increased risk for mortality.
Finally, our findings confirmed that steroids are associated with survival benefit in our patients, consistent with the (RECOVERY) (Randomized Evaluation of Covid-19 Therapy) trial. Steroid therapy decreases the inflammatory response contributing to the severity of the illness. That’s why it’s essential that it’s readily available for critically ill COVID-19 patients.
Urgent next steps
This study has two important implications for policymakers.
Firstly, there is the immediate response. It is critical that vaccination is made a priority. Vaccination is an important intervention when it is impossible to provide safe and adequate critical care across the continent.
Vaccine inequality cannot be accepted, and it is important to accept that ‘we are not safe, until we are all safe’. It would be devastating to see a scenario similar to India play out in Africa due to insufficient vaccination.
The second response for policymakers is a more long term strategy. Certainly, the data from the study suggest that regulations are needed for minimum resource requirements for critical care provision in Africa. The study shows that there is a need for a substantial increase in resources needed to provide an acceptable quality of critical care in Africa.
Lastly, we are very aware that the situation is more dire than the study shows. This is for two reasons.
The first is that only 10 countries out of 40 that were initially invited took part in the survey. It’s likely that the countries that did’t take part didn’t have the capacity to participate because of the demand on their clinical service delivery during the pandemic. And it’s likely that these sites may have worse outcomes than reported in the study.
Secondly, the participating hospitals were predominated by university and tertiary hospitals. These are better resourced than critical care units in hospitals of a lower level. They are, therefore, in a better position to provide more comprehensive care, with possibly better outcomes than non-participating sites.
In conclusion, outcomes for critically ill COVID-19 patients in Africa are poorer than any other region in the world. This is driven by resource-poor facilities. As long as the population of Africa remains unvaccinated, this has the potential for a catastrophic loss of life in Africa.![]()
Bruce M Biccard, Professor and Second Chair at Groote Schuur Hospital , University of Cape Town.
UCT’s response to COVID-19 in 2021
COVID-19 is a global pandemic that caused President Cyril Ramaphosa to declare a national disaster in South Africa on 15 March 2020 and to implement a national lockdown from 26 March 2020.
UCT is taking the threat of infection in our university community extremely seriously, and this page will be updated regularly with the latest COVID-19 information. Please note that the information on this page is subject to change depending on current lockdown regulations.

Global Citizen Asks: Are COVID-19 Vaccines Safe & Effective?
UCT’s Institute of Infectious Disease and Molecular Medicine (IDM) collaborated with Global Citizen, speaking to trusted experts to dispel vaccine misinformation.
If you have further questions about the COVID-19 vaccine check out the FAQ produced by the Desmond Tutu Health Foundation (DTHF). The DTHF has developed a dedicated chat function where you can ask your vaccine-related questions on the bottom right hand corner of the website.
IDM YouTube channel | IDM website
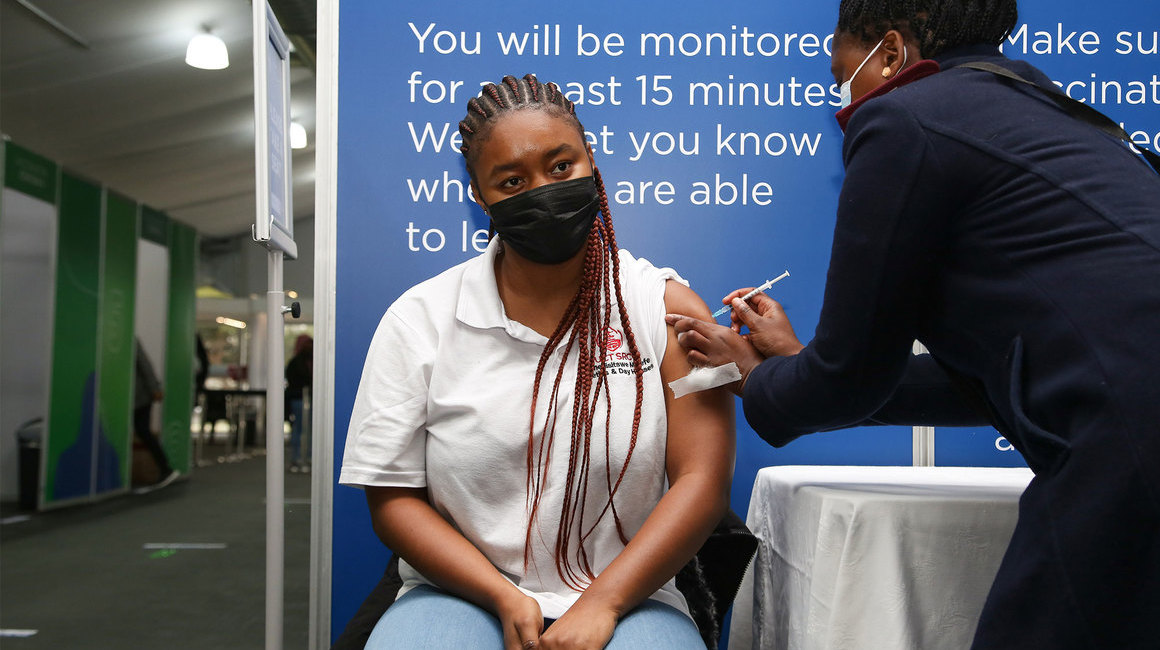
UCT Community of Hope Vaccination Centre
The University of Cape Town in partnership with the Western Cape Government (WCG) have reinforced our commitment to bringing hope to the residents of the Mother City with the launch of the world‑class Community of Hope Vaccination Centre that opened its doors on Monday, 30 August 2021.
The site is located on Main Road in Mowbray – in the Forest Hill Residence – and access is from Broad Street. The site is open every Monday to Friday from 08:00 to 15:00 and on Saturday from 09:00 to 13:00. Please allow time for attending to COVID-19 protocols and arrive as early as possible at the vaccination centre.
Frequently asked questions
News and views
Campus communications
2021
Media releases
Read more
UCT statements related to COVID-19 vaccinations
This is a space created for all formal bodies and structures within the university community to share their opinions on the need for a mandatory COVID-19 vaccine policy. Please note that some editorial judgement may be applied if the received statements go against any constitutional rights, and that no correspondence will be entered into, statements will be posted unedited and as received. Statements can be sent to opinions@uct.ac.za.
Commemorating a year of COVID-19
At midnight on 26 March 2020, South Africa went into the first nationwide hard lockdown. A year later, we remember those who have died and those who have been affected by COVID-19, as well as the pandemic’s effects across society and campus. We are especially grateful for the front-line health workers who have done so much for so many.
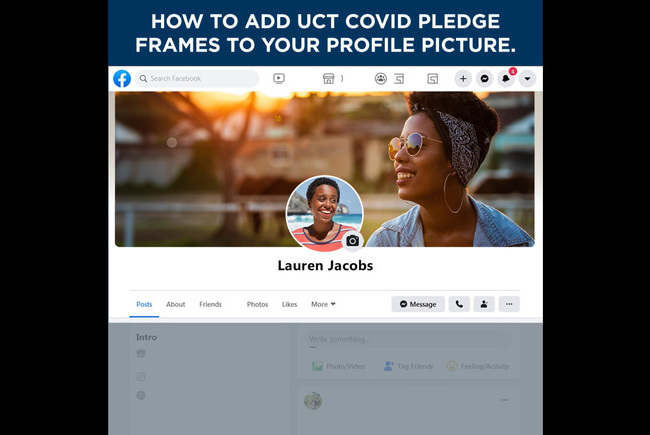
#UCTCOVIDPledge – social media elements
Customised Facebook frames and Instagram stickers are now available on those social media platforms. Watch the tutorial videos here to see how easily you can show your support for the #UCTCOVIDPledge.
In an email to the UCT community, Vice-Chancellor Professor Mamokgethi Phakeng said:
“COVID-19, caused by the virus SARS-CoV-2, is a rapidly changing epidemic. [...] Information [...] will be updated as and when new information becomes available.”
We are continuing to monitor the situation and we will be updating the UCT community regularly – as and when there are further updates. If you are concerned or need more information, students can contact the Student Wellness Service on 021 650 5620 or 021 650 1271 (after hours), while staff can contact 021 650 5685.