Emergency medicine team rises above the challenges
18 August 2020 | Story Kim Cloete. Photo Getty Images. Read time 8 min.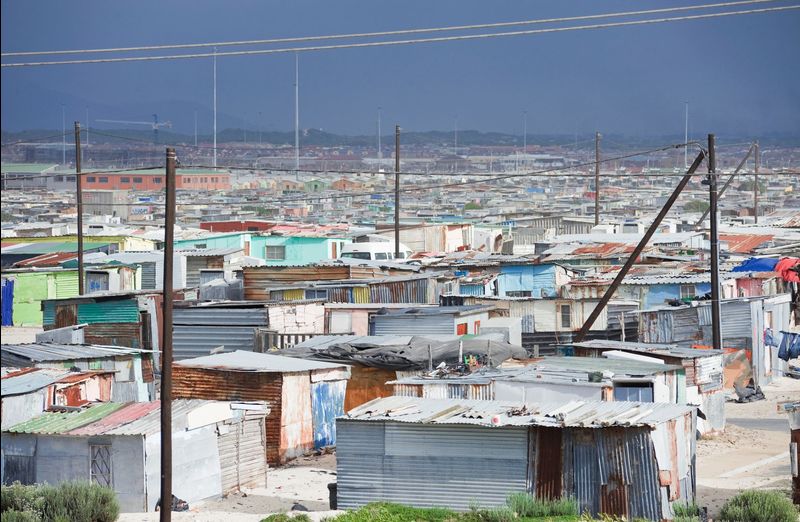
A tightly knit team of University of Cape Town (UCT) emergency medicine specialists have overcome multiple challenges and set up a dynamic system to cope with the wave of COVID-19 patients at the busy Mitchells Plain District Hospital and the Heideveld Emergency Centre in Cape Town.
“COVID-19 brought the perfect storm. We have a low-resource setting with limited staff. Then we had a situation that involved mortality, lots of fear and stigma, and where staff were separated from their support base and families,” explained Dr Clint Hendrikse, an emergency physician.
But instead of being disheartened by the obstacles, the team of emergency physicians surged ahead with new ways of doing things, forging much-needed contact between patients and their families and handling the rising COVID-19 infections, which peaked at the end of June.
Preparation was key
Hendrikse believes preparation made a huge difference to how they were able to stay on top of the situation.
Apart from big hospitals like Groote Schuur and Tygerberg, the Mitchells Plain District Hospital has had the highest number of COVID-19 admissions in the Western Cape and is the busiest emergency centre in the province – it covers a population of 700 000.
When the first signs of COVID-19 appeared in South Africa, the five-member team of emergency physicians, who are joint staff at UCT, buckled down.
Oxygen, space and staff
In between dealing with emergencies, like heart attacks and trauma, they created dedicated COVID-19 wards and planned the three essential elements to tackle the coronavirus – “oxygen, space and staff,” said Hendrikse.
“We are a district-level hospital, so [we] don’t have an intensive care or high-care unit. We literally had to create an [intensive care unit] ICU from scratch, train staff and put systems in place.”
The initial three-week countrywide lockdown bought them valuable time, said emergency physician Dr Martin de Man.
“We chose to split the emergency centre into two sections at the Mitchells Plain [District] Hospital to separate COVID-19 patients from other patients and to ensure that we kept our staff safe.”
It also involved separating the paediatrics ward and making changes to the Heideveld Emergency Centre. Ultimately, six emergency centres were formed instead of the usual two.
“We also established very early [on] that we would need to work very closely with our Department of Medicine colleagues after stabilising patients,” said De Man.
Testing tent staffed by nurses
At the same time, emergency physician Dr Katya Evans set up a screening and testing tent alongside the Mitchells Plain District Hospital. She is particularly proud that the tent has been completely staffed by nurses.
“The nurses were initially afraid to test patients. It was a totally new experience for them, but we spent two solid weeks on training and it paid off. It is one of the few tents that are nurse-driven, but they have been empowered. They did, and continue to do, an amazing job. So far we have tested, well, about 10 500 people.”
“It is one of the few tents that are nurse-driven, but they have been empowered.”
As of 14 August 2020, 3 593 out of the 10 500 people tested positive for COVID-19, and the Mitchells Plain District Hospital had admitted 1 659 COVID-19-positive patients, of which 182 have died.
For the team, one of the crucial aspects was communication.
“Initially the National Institute for Communicable Diseases (NICD) was managing the numbers of COVID-19 cases, but when numbers skyrocketed, contact tracing teams became overwhelmed and the thousands of queries became a daunting task,” said Hendrikse.
Undeterred, and working closely with the NICD and the health authorities, Evans set up a groundbreaking electronic system to manage the results. It pulls all the results of patients that have been tested, informs them of their results and gives them advice.
Connecting patients with their families
Flowing from this, emergency physician Dr Candice van Koningsbruggen was instrumental in connecting patients with their families, who were desperate for information and to have some kind of contact.
“Visitors weren’t allowed at the hospital. The last time a family would see their loved one was at the entrance to the hospital, and often not again for days and weeks.”
Thanks to mobile devices donated by a doctor-led organisation called Masks for Medics, medical teams were able to arrange calls or video calls between patients and their family members. Doctors would also call the families if patients were too sick to make the call themselves. A community liaison nurse would also update each family at least once a day. This lifeline was of great comfort to patients and their families.
Support and a sense of purpose
It was also vital to build a culture of care and support for the 40 doctors and staff at the hospital.
“One of the things we are proudest about is our teamwork. All our doctors work beautifully together with their teams and within specialities within the hospital,” said Van Koningsbruggen. Everyone from anaesthetists to gynaecologists offered their time and formed part of the greater COVID-19 team which would oversee patients.
Hendrikse concedes that there was heartbreak and tears along the way as staff members had to deal with death and dying, as well as being separated from their children and families, often for months, to prevent the spread of infection. But they offered as much support as they could and arranged counselling sessions for staff who had COVID-19 symptoms, who tested positive or were isolated from their families.
“One of the things we are proudest about is our teamwork. All our doctors work beautifully together with their teams.”
Van Koningsbruggen said waking up with a purpose every day also propelled them forward.
“We are here because we love our patients and we love what we do. That situation helped us thrive.”
Hendrikse believes their experience in the often very tough and stressful world of emergency medicine also helped the team.
“To work as an emergency physician, you have to have a strong internal drive. That pulled us through … and when staff saw patients getting better, they realised they were doing a great service to the community.”
Lessons learnt
While the number of patients has halved compared to what it was at the peak of the crisis, the emergency physicians haven’t dropped their guard. They’re also learning valuable lessons along the way.
“From an operational point of view, we’ve learnt a lot about the potential design and layout of emergency centres in the case of a pandemic. From an infection control point of view, we’ve learnt lessons that we can use in how we manage tuberculosis,” said Hendrikse.
Community screening has been very effective. Hendrikse sees opportunities for screening in the community for hypertension, diabetes and other chronic conditions.
Beyond the practical learnings, the team has also learnt the value of appreciating the work of staff – from porters and doctors to cleaners and nurses. The support shown to staff cascaded to the patients, as nurses would encourage patients and often sing to them. Even a 20-second song timed with the 20-second handwashing ritual formed part of their repertoire.
“When our system came under strain, we worked longer and harder. COVID-19 has opened our eyes to what we are capable of,” said Hendrikse.
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.
UCT’s response to COVID-19
COVID-19 is a global pandemic that caused President Cyril Ramaphosa to declare a national disaster in South Africa on 15 March 2020 and to implement a national lockdown from 26 March 2020. UCT is taking the threat of infection in our university community extremely seriously, and this page will be updated with the latest COVID-19 information. Please note that the information on this page is subject to change depending on current lockdown regulations.
Minister of Health, Dr Joe Phaahla, has in June 2022 repealed some of South Africa’s remaining COVID-19 regulations: namely, sections 16A, 16B and 16C of the Regulations Relating to the Surveillance and the Control of Notifiable Medical Conditions under the National Health Act. We are now no longer required to wear masks or limit gatherings. Venue restrictions and checks for travellers coming into South Africa have now also been removed.
Read the latest document available on the UCT policies web page.
Campus communications
2022
UCT Community of Hope Vaccination Centre
On Wednesday, 20 July, staff from the University of Cape Town’s (UCT) Faculty of Health Sciences came together with representatives from the Western Cape Government at the UCT Community of Hope Vaccination Centre at Forest Hill Residence to acknowledge the centre’s significance in the fight against COVID-19 and to thank its staff for their contributions. The centre opened on 1 September 2021 with the aim of providing quality vaccination services to UCT staff, students and the nearby communities, as well as to create an opportunity for medical students from the Faculty of Health Sciences to gain practical public health skills. The vaccination centre ceased operations on Friday, 29 July 2022.
With the closure of the UCT Community of Hope Vaccination Centre, if you still require access to a COVID-19 vaccination site please visit the CovidComms SA website to find an alternative.
“After almost a year of operation, the University of Cape Town’s (UCT) Community of Hope Vaccination Centre, located at the Forest Hill residence complex in Mowbray, will close on Friday, 29 July 2022. I am extremely grateful and proud of all staff, students and everyone involved in this important project.”
– Vice-Chancellor Prof Mamokgethi PhakengWith the closure of the UCT Community of Hope Vaccination Centre, if you still require access to a COVID-19 vaccination site please visit the CovidComms SA website to find an alternative.
Frequently asked questions
Global Citizen Asks: Are COVID-19 Vaccines Safe & Effective?
UCT’s Institute of Infectious Disease and Molecular Medicine (IDM) collaborated with Global Citizen, speaking to trusted experts to dispel vaccine misinformation.
If you have further questions about the COVID-19 vaccine check out the FAQ produced by the Desmond Tutu Health Foundation (DTHF). The DTHF has developed a dedicated chat function where you can ask your vaccine-related questions on the bottom right hand corner of the website.
IDM YouTube channel | IDM website
“As a contact university, we look forward to readjusting our undergraduate and postgraduate programmes in 2023 as the COVID-19 regulations have been repealed.”
– Prof Harsha Kathard, Acting Deputy Vice-Chancellor: Teaching and Learning
We are continuing to monitor the situation and we will be updating the UCT community regularly – as and when there are further updates. If you are concerned or need more information, students can contact the Student Wellness Service on 021 650 5620 or 021 650 1271 (after hours), while staff can contact 021 650 5685.