UCT Family Medicine registrars experience new ‘Hospital of Hope’
06 July 2020 | Story Thania Gopal. Photos Supplied. Voice Sarin Drew. Read time 9 min.
Just a few months ago, Dr Abhaya Karki and Dr Nabeela Amien, two senior family medicine registrars from the University of Cape Town (UCT), could not have imagined being part of a team that would set up a field hospital from scratch – from preparing beds to welcoming the first patients and leading one of the multidisciplinary teams who look after acutely ill COVID-19 patients. The duo have described it as “the experience of a lifetime”.
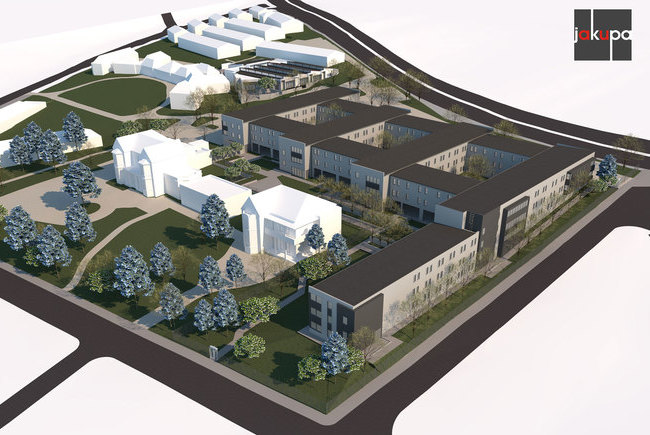
The aptly named Hospital of Hope sprang up in a matter of weeks when the Cape Town International Convention Centre (CTICC) was repurposed into an 862-bed field hospital. This was done as part of the Western Cape Government’s health strategy to increase capacity to mitigate the impact of the COVID-19 pandemic on its communities.

After weeks of preparation, the facility was officially opened by the president of South Africa, the minister of health and the premier of the Western Cape on Friday, 5 June 2020. The facility received its first patients from other acute hospitals on Monday, 8 June 2020.
“Our daily activity begins with a huddle in the morning, laying out the plan for the day. The CTICC has a high turnover of patients, so we have lots of discharges to sort out in the morning; we try to sort them out first. We also see our sickest patients and then carry on with new admissions and stable patients,” said Karki.
Along with Amien, he is part of a team of eight clinical team leaders responsible for managing doctors at the facility and for providing patient care.
Providing high-quality care
In order to fulfil its vision of “providing high-quality, team-based person-centred care”, Associate Professor Klaus von Pressentin, head of the Division of Family Medicine, said the clinical teams are multi-disciplinary in nature with a strong family medicine focus. They include nurses, physiotherapists, dietitians, social workers, radiographers and pharmacists.
“The biggest success that this team has had is that of starting something from scratch and managing to keep it running successfully with incredibly high standards of care. COVID-19 is a disease that can bring about anxiety and fear in even the strongest-minded clinicians, yet at the CTICC Hospital of Hope patients are still treated with compassion and respect. The amount of passion I have seen from the staff is absolutely incredible,” said Amien.
“The amount of passion I have seen from the staff is absolutely incredible.”
The facility’s care package, said Von Pressentin, is tailored to patients diagnosed with moderate COVID-19 disease in need of inpatient oxygen therapy whose disease profile is complicated with existing chronic conditions, and patients with a care plan which is predominantly focused on palliative care.
Karki said that while it is hard to measure success under such trying circumstances, he really values patient feedback.
“The smile [on the patient’s face] makes me think that we are doing good. These patients are referred from busy facilities. When they arrive here in a big dome, they don’t know what to expect – and then they see caring people, people who are not afraid to talk to them, to take them to the toilet, to clean them … and they feel at ease. They don’t feel alienated. This is purely anecdotal, but I have [had] many patients tell me about the pleasant experience. It makes the whole journey worth the travel.”
All hands on deck
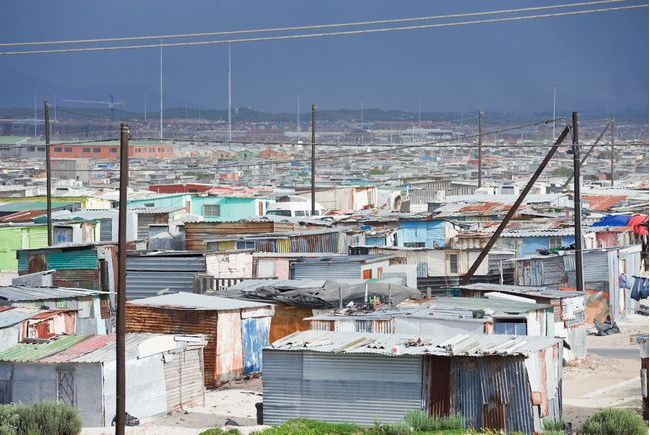
The Hospital of Hope facility is staffed by health workers from diverse backgrounds: Cuban health workers, as well as South African health workers who were recruited from the private sector, deployed from existing posts in the public health system and/or local higher education institutions.

A number of divisions within UCT’s Faculty of Health Sciences have also contributed to this project, including Emergency Medicine, Family Medicine and the Primary Health Care Directorate. Professor Lee Wallis and his emergency medicine team have helped plan the intermediate care facilities during the commissioning phase and are managing the interfacility transfer processes and acute facilities’ bed bureau.
Von Pressentin and Dr Tasleem Ras have been assigned as clinical managers of the facility. They are supported by a strong clinical team, which includes several family physicians and family medicine registrars. Professor Steve Reid from the Primary Health Care Directorate has joined the team to help facilitate interprofessional learning conversations and create a learning culture.
Challenges
One of the biggest challenges faced by health workers at the facility is the fear of not being able to cope with the vast number of patients. Amien said the influx of patients will result in strain among the staff and may lead to high levels of burnout.
“For this reason, it is very important that we put in place measures that ensure that we work as efficiently as possible. Staff can also remain motivated by sharing success stories, as well as positive messages from other patients and staff. It is also important to let staff know that they are appreciated.”
Karki said the hardest part is having to communicate with families after they have lost a loved one.
“Due to the nature of this disease, family members are not allowed to be with patients. It is an uncomfortable and heartbreaking phone call we have to make. Dealing with our emotions under such circumstances is challenging.”
“Dealing with our emotions under such circumstances is challenging.”
The value of teamwork
Karki described the camaraderie between health workers as a huge asset.
“We support each other. We value each other and deep down knowing that all of us have volunteered to be here and serve is a humbling feeling. I use humour to support my group. We laugh, and when we cry, we cry together. But we communicate with each other. I always ask them how [they are feeling] – just to get an idea [of where they are emotionally].”
Experiencing a pandemic first-hand has also provided a steep learning curve for the family medicine registrars, who have realised the importance of teamwork and have used this opportunity to reflect and improve on their interpersonal skills.
“I was working as a registrar in my pre-COVID life and now I work as a consultant to a group of very involved medical officers. We also have senior Cuban doctors in the mix. We learn from each other,” Karki said.
“I guess for me the biggest learning opportunity that this unprecedented event has offered is the leadership. I now have a clearer picture of my strengths and weaknesses as a leader. My team feels comfortable around me; we have discussions and we try to resolve things without conflict.”

Amien said she feels more confident in her abilities to manage and lead the clinical teams.
“It is important to bear in mind that we still have a lot to learn and to always be willing to hear what someone else has to say. I have enjoyed working with other members of the multidisciplinary team. These relationships have been really special and have shown me the importance of teamwork.”
For Amien, the greatest satisfaction has come from her interactions with patients and their families.
“Video calling families daily has been an incredibly rewarding experience. For most of my patients I do daily video calls and … the relationship and bond that you form with these family members are amazing,” she said. “Even though family can’t come visit, these video calls have provided a special form of family-orientated care that I have not experienced before, but is probably even stronger than meeting families once-off.
“I cannot overemphasise how much these calls mean to the patients … I consistently have seen sad and forlorn patients lying in their beds and as soon as the video call gets made, it is like they are a new person. I have never seen such huge smiles! This has undoubtedly become the favourite part of my day and I plan to take this away with me when I leave the CTICC to implement in my practice.”
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.
Highlights from 2020
As we look back on 2020, we celebrate some of the stories that were popular with readers of the UCT News website during the year.

UCT marked a historic moment on its journey of transformation when it launched the Khoi and San Centre on 21 September.
11 Jan 2021 - >10 min read Highlight from 2020
In September, over 30 members of the UCT community were honoured in the Mail & Guardian 200 Young South Africans list.
08 Jan 2021 - 9 min read Highlight from 2020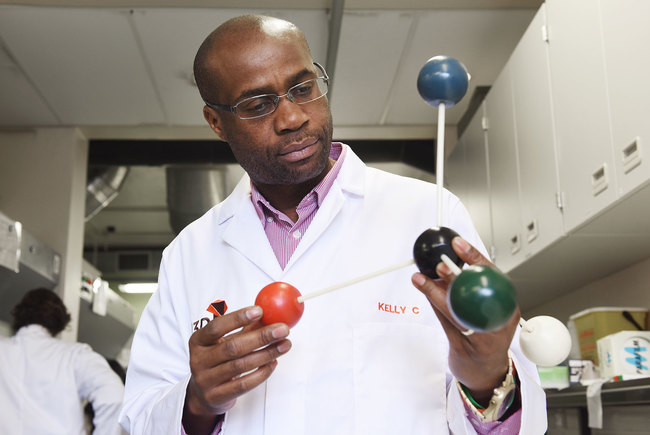
In April, UCT’s Professor Kelly Chibale was chosen as one of the world’s top 60 inspirational leaders in the pharmaceutical industry.
23 Dec 2020 - 7 min read Highlight from 2020
In April 2020, women took four of the five top spots in the final-year civil engineering class, a salute to excellence and a spur to equality.
22 Dec 2020 - >10 min read Highlight from 2020
The Mamokgethi Phakeng Scholarship was launched in 2020 to support young black women in STEM fields of study at UCT.
21 Dec 2020 - 9 min read Highlight from 2020