New antimalarial compound could stave off threat of drug-resistant malaria
16 May 2017 | Natalie Simon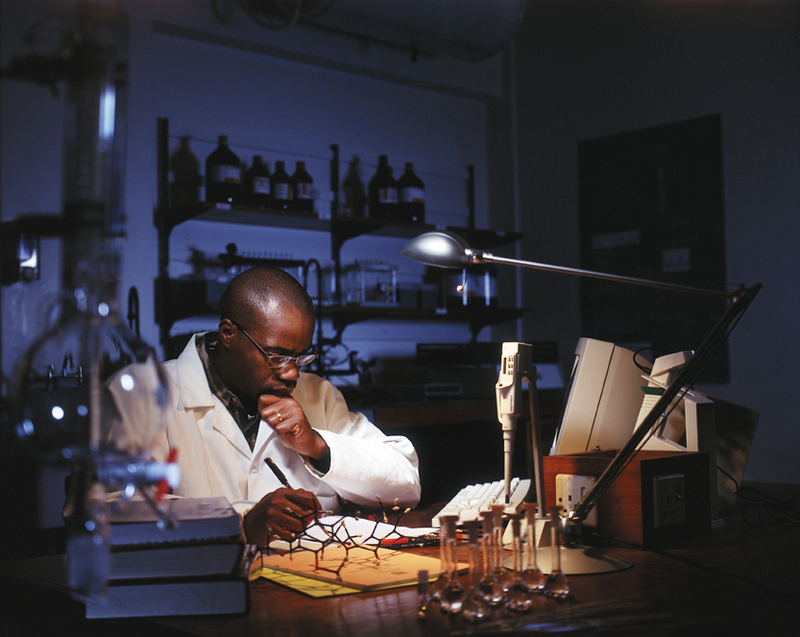
Humans have been affected by malaria for thousands of years, according to the Center for Disease Control and Prevention. References to malaria or a disease resembling malaria can be found in ancient Chinese writings dating back to 2700 BC, and malaria is believed to be responsible for the decline of city-state populations in the 4th century BCE Greece. Over the millenia, humans have discovered and developed plants and compounds to treat malaria – but the parasites that cause malaria have continually outwitted us by evolving resistance to malaria treatments.
As a result, malaria remains one of the world’s biggest killers, with 212 million new malaria infections reported in 2015 and nearly half a million deaths in the same year, according to the World Health Organisation. Ninety-two percent of those deaths occurred in Africa.
Today scientists argue that resistance to anti-malarial drugs is one of our biggest challenges when it comes to both malaria control and eradication. Malaria parasites are very diverse genetically and are constantly mutating to respond to environments. Parasites that evolve beneficial mutations, such as resistance to drug treatments, then pass these mutations on to the next generation of parasites, spreading the drug resistance and making existing drugs less efficient and/or useless against the disease.
A totally novel mechanism to treat malaria
This is one of the reasons why the recent discovery and biological profiling of antimalarial clinical drug candidate by the Drug Discovery and Development Centre (H3D) and MMV in collaboration with international researchers, under the leadership of Professor Kelly Chibale, is so significant. This compound, known as MMV390048 (also known as MMV048), belongs to an entirely new chemical class and uses a novel mechanism to kill the malaria parasite.
“The mechanism by which this new compound works has never been seen or used before in a clinical setting,” says Chibale, “which means that, at this stage, no malaria parasites have developed any kind of resistance to this compound in a clinical setting.”
Effective at all lifecycle stages of the malaria parasite
A significant portion of the malaria parasite’s lifecycle takes place inside the human body. When a malaria-carrying anopheles mosquito bites a person, it transfers malaria parasites into the human bloodstream through its salivary glands. These parasites then travel to the liver cells where they multiply. Eventually, the liver cells rupture and release the parasites back into the blood, where they invade the red blood cells and rupture those cells too.
It is in the red blood cells that the parasite develops into male and female reproductive cells, which are then transferred to the next mosquito that happens to come along and bite a malaria-infected human, starting the whole cycle again in another body.
According to YourGenome.org, in the current malaria treatment regimen, different drugs target different stages of the parasite lifecycle. This means that drugs often need to be used in combination to ensure the parasite is removed from all areas of the body. If any parasites are left in the body after treatment, the disease can return months – or even years – later.
MMV048 is one of the few antimalarial compounds in development that is effective across the entire lifecycle of the parasite.
“The ability of MMV048 to block all lifecycle stages of the malaria parasite, offer protection against infection as well as potentially block transmission of the parasite from person to person, suggests that this compound could contribute to the eradication of malaria, a disease that claims the lives of several hundred thousand people every year,” says Chibale.
Single-dose treatment
Another unique element of MMV048 is its potential as a single-dose treatment, which, according to Dr David Reddy, chief executive officer of MMV, could revolutionise malaria treatment.
According to Chibale, existing malaria treatments involve taking multiple doses of medicines daily for three or four days. The potential for a single dose is thus a game-changer, as it would reduce the chance that patients will forget to take their medicine or take it at the wrong times. It makes it easier for healthcare practitioners to ensure patients take their medication through direct observation – and, significantly for Africa, it reduces many of the costs associated with treatment. This also makes the treatment regimen far more manageable, especially in rural and underresourced areas.
MMV048 ready for Phase IIa human trials
In 2014, MMV048 became the first new antimalarial medicine to enter phase I human studies in Africa. Today, preparations are being made to begin phase IIa human trials on this promising compound as a single-dose cure.
The phase I trials – referred to as “first-in-man studies” – are, as the name suggests, the first testing of a compound on human subjects. They will generally involve a small group of between two and 100 volunteers and are designed to determine in what quantities a drug can be administered. Phase II trials are conducted on larger groups (between 100 and 300) and are designed to show clinical efficacy or biological activity of the drug.
“With a demonstrated three-in-one profile of potentially offering protection, achieving single-dose cure and blocking transmission, this compound has the potential to revolutionise the treatment of malaria if it successfully goes through the remaining stages of human clinical trials and gets regulatory approval,” says Chibale.
H3D have a second potent anti-malarial candidate in the works

In July 2016, H3D identified a new potent anti-malarial development candidate with potential for both treatment and prevention of malaria.
The compound, referred to as UCT943, was the second preclinical candidate to come out of the collaboration led by H3D involving the Switzerland-based Medicines for Malaria Venture (MMV) and an international network of partners.
Developed to strengthen the parasite enzyme phosphoinositide 4-kinase inhibitor programme, UCT943 has the same molecular target as MMV048, a promising new compound researched by an international team led by H3D and selected for development in 2012. The data so far shows that UCT943 has promise to be more potent against the parasite, and to be easier to formulate, although these aspects will be the subject of the next studies, and ultimately will need to be validated in humans.
“Like MMV048, UCT943 has potent activity against all stages of the malaria parasite life-cycle and has the potential to block transmission of the parasite from person to person and, as such, could contribute to the eradication of malaria, a disease that claims the lives of around half a million people every year,” said Chibale, at the time of the announcement.
UCT Vice-Chancellor, Dr Max Price, said: “Delivering two preclinical candidates within five years is an outstanding record by international standards especially for a drug discovery centre based at an academic institution. The value of a second candidate signals that the first compound was not a once-off, but part of a sustained and systematic programme.”
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.









