Status epilepticus: New research on failing meds
09 October 2019 | Story Helen Swingler. Photos Joseph Raimondo. Read time 7 min.
A new paper by University of Cape Town (UCT) researchers and their international co-authors has explained why patients experiencing unrelenting epileptic seizures, or status epilepticus, stop responding to first-line medication benzodiazepine.
The just-published paper in the journal Brain: A Journal of Neurology not only describes the mechanism underlying benzodiazepine resistance in patients but also illustrates how, in certain situations, the drug actually exacerbates seizures, said corresponding author Dr Joseph Raimondo, a senior lecturer in the Division of Cell Biology.
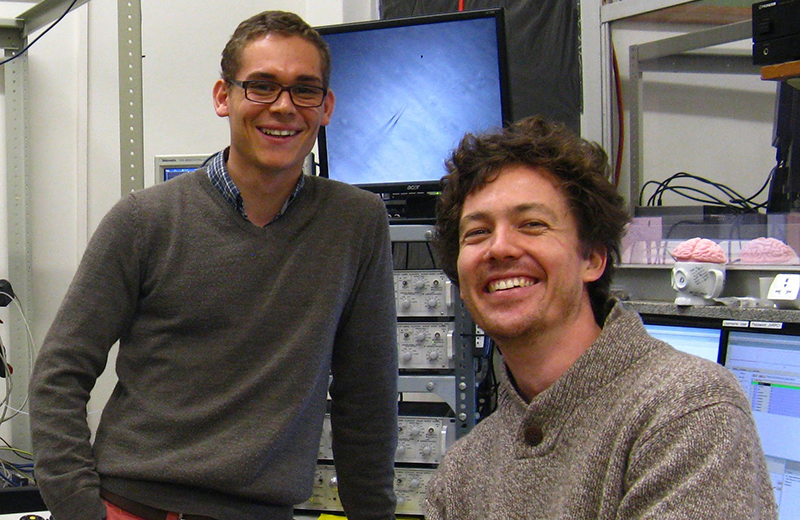
Raimondo’s former master’s student Richard Burman is lead author among a long line of international contributors from Oxford and Newcastle universities. Since its establishment in 1878 Brain has published landmark papers in clinical neurology and translational neuroscience.
Epileptic seizures are caused by “electrical storms” or bursts of electrical activity in the brain. Most seizures stop within minutes. But status epilepticus is characterised by unrelenting seizures and is a serious condition that can cause brain damage. It also has a high mortality rate.
Until now, benzodiazepines have been the first-line therapeutic treatment for status epilepticus. But in many cases this drug is ineffective.
“As benzodiazepines works in less than 50% of cases, it means we really should think about other strategies to stop these seizures,” said Raimondo.
Their breakthrough discovery is expected to improve the management of this condition in clinical settings and point the way ahead in terms of new therapies. For example, they showed that a different drug, phenobarbital, is very effective. Currently however, the drug is hard to come by as it is not profitable for drug companies.
Developing world problem
Epilepsy is the most common neurological disease in the world. But it is far more common in the developing countries of the global south, especially in Africa because of the region’s higher rates of brain trauma and brain infections. The latter are the main causes of status epilepticus.
The research underpinning the paper was done in collaboration with Professor Jo Wilmshurst, head of paediatric neurology at the Red Cross War Memorial Children’s Hospital, who provided the clinical data. Burman split his time between the hospital’s emergency room and Raimondo’s laboratory.
“Part of the study was with these child patients who have these seizures that don’t stop by themselves,” said Raimondo.
The researchers found that 48% of the children with status epilepticus did not respond to treatment with the drug and, critically, that the duration of seizures before treatment was administered was an important predictor of non-responsiveness.
It was back to the laboratory where Raimondo and Burman had, over six years, built up the sensitive equipment for the cutting-edge techniques they needed to study miniscule individual brain cells. Some equipment was donated by colleagues overseas and grants bought other equipment which the duo built or assembled themselves. None of this capability existed in Africa prior to this work.
“The techniques are quite cool,” said Raimondo, who has always enjoyed tinkering with things mechanical.
“We looked at how brain cells talk to one another during these seizures and what goes wrong in the signalling, and then added the drugs to observe what they do – and why they don’t work.”
“The better your equipment is the deeper you can see into the biological world. So, if you enjoy constructing machines that can help you understand the science you can do more exciting things.”
He’s particularly pleased that their techniques have been homegrown to generate research that’s relevant to the African context, but also extremely relevant throughout the world.
Using rodent brain slices, the duo studied the cellular mechanisms in the brain that underlie acquired benzodiazepine resistance.
“We looked at how brain cells talk to one another during these seizures and what goes wrong in the signalling, and then added the drugs to observe what they do – and why they don’t work,” he explained.
Laboratory techniques
The first laboratory technique they used is patch clamp electrophysiology, used to study ionic currents in individual, isolated living cells, tissue sections, or patches of cell membrane.
“Robotic arms place tiny electrodes onto the miniscule brain cells so we can record the electrical signalling.”
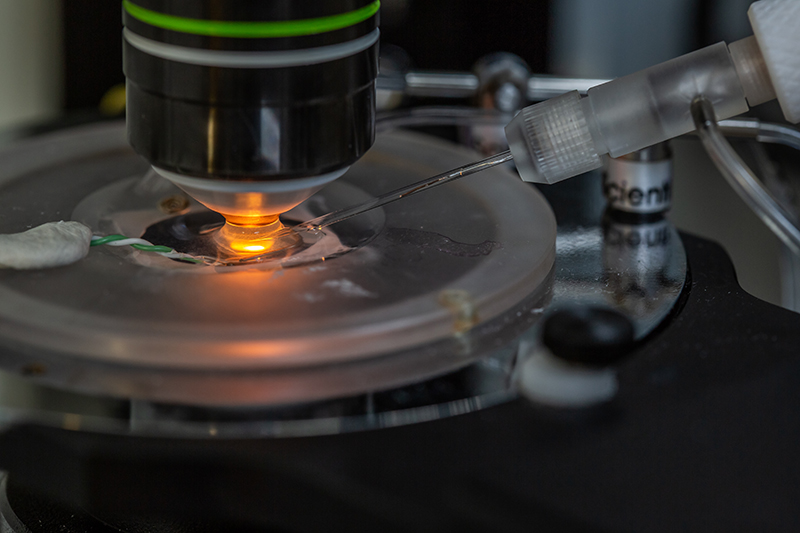
The second used optogenetics, a biological technique that involves the use of light to control cells in living tissue, typically neurons, that have been genetically modified to express light-sensitive ion channels. Here they controlled certain brain cell activity in genetically engineered mice with light.
“Basically, you shine light on the brain cells and then you control the brain cells and record how they talk to each other electrically. We use that to show that the cells that are normally inhibitory during a seizure that doesn’t stop become excitatory instead.”
“Most of our experiments were done on animal brain slices; it’s a leap from there to the clinic so we have to be very cautious about how we interpret our findings.”
The other technique involved “fancy microscopes” to directly measure chloride concentrations in the neurons in the brain cells. This proved pivotal to the study as chloride ions affect gamma-aminobutyric acid (GABA), a neurotransmitter that’s widely distributed in the neurons of the brain cortex. Its main role is reducing neuronal excitability in the nervous system, and it also controls anxiety.
Explaining the link to seizures, Raimondo said: “The longer the seizure, the more chloride ions flow into the neurons in the brain cells. When this happens the action of GABA changes from being inhibitory to becoming excitatory. Because benzodiazepine drugs activate GABA receptors, instead of calming brain cells and stopping seizures, they excite the neurons and make the seizures worse.
“And that’s the secret to it.”
Africa-specific
His lab also studies causes of seizures that are particular to Africa, such as neurocysticercosis, caused by tape worm larvae in the brain – the biggest cause of acquired epilepsy globally.
“But it’s very understudied because it doesn’t really exist in the Western world.”
Where to now?
The next step is to work with clinicians to begin thinking about different clinical approaches and strategies for treating unrelenting epileptic seizures, said Raimondo.
“Most of our experiments were done on animal brain slices; it’s a leap from there to the clinic so we have to be very cautious about how we interpret our findings.”
- Burman completed his MMed in Raimondo’s laboratory while studying towards his MBChB.
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.










