Developing immunotherapies relevant to Africa
02 May 2019 | Story Neelakshi Mungra, Krupa Naran and Trishana Nundalall. Photo DarkoStojanovic, Pixabay. Read time 7 min.
The exorbitant costs of cancer drugs make it difficult for public and private health care systems to provide the latest treatments to patients. If this trend continues it will become increasingly difficult for patients to access basic cancer treatment, let alone the new generation of immunotherapy drugs.
Immunotherapy refers to a therapeutic approach that targets or manipulates the immune system to fight disease without harming normal cells.
Most cancer research has been done on populations of European descent. This means that there’s minimal data on African populations.
In March 2019, the US released the first immunotherapy drug for breast cancer to be approved by the Food and Drug Administration. The drug, called Tecentriq, is used to treat triple-negative breast cancer. This type of cancer is resistant to surgery and chemotherapy. It highlights the major benefits of immunotherapy in patients who have limited – if any –treatment options.
For developing countries like South Africa, finding immunotherapy solutions is particularly important given the country’s weak health system and the high cost of cancer drugs. The University of Cape Town has set up the country’s first such laboratory, the Medical Biotechnology and Immunotherapy Unit (MB&I), led by Professor Stefan Barth. The lab, where we do our research, is strongly committed to the development of novel therapeutic and diagnostic tools for cancer.
Most cancer research has been done on populations of European descent. This means that there’s minimal data on African populations. Our lab aims to fill this knowledge gap by diagnosing and treating patients of African descent. The aim is to identify immunotherapy targets in this underrepresented population.
Our research
There are five main classes of immunotherapies. These are:
-
Cancer vaccines: These are a collection of immune cells that have been removed from a cancer patient and manipulated to enhance their ability to attack cancer before being readministered into the patient.
-
Cytokine immunotherapy: This involves treating a patient with cytokines, which are proteins made by immune cells that signal other immune cells to kill a cancerous cell.
-
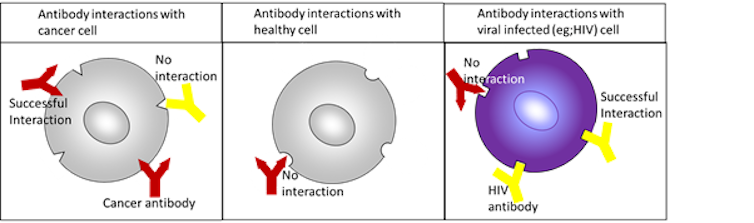
Antibody-based therapies: These represent the largest class of approved immunotherapies and are our lab’s main research focus. Antibodies are proteins produced by the body’s immune cells. These can identify pathogens and elicit a response to eradicate diseased cells or disease-causing agents.
Antibodies are like puzzle pieces – and diseases are like an incomplete puzzle. Therefore, only antibodies with a specific shape will fit into the “cancer puzzle”. Antibodies with other shapes would fit other puzzles, but not cancer. The ability of antibodies to discriminate between different cells and diseases is the basis for antibody-based immunotherapies.
Our current research involves attaching a light detectable agent to the puzzle piece. This allows us to visualise where a cancer cell is located in a cancer patient’s tissues. We can characterise different types of cancer cells by attaching different coloured light detectable agents to different antibodies. We then generate antibody-drug conjugates that deliver the drug directly to the cancer without harming healthy cells by replacing the light detectable agent on a cancer-fitting antibody with a toxic drug.
-
Immune checkpoint inhibitors: These are essentially antibodies that target specific proteins on tumour cells or T-cells (the main immune cells responsible for killing cancer). These proteins normally send inhibitory signals from cancer cells to T-cells, resulting in T-cell inactivation. By interfering with this signalling, immune checkpoint inhibitors allow T-cells to be activated and tumour cells to be killed.
-
Adoptive cell therapies: These include the popular CAR-T cell therapies that enhance the natural ability of T-cells to fight cancer. Similar to antibodies, T-cells express different “puzzle pieces” on their surface. These allow them to attach to an incomplete diseased puzzle and to then kill the disease. CAR-T cells are T-cells that have been removed from a patient and modified to have a cancer-specific puzzle piece, allowing the T-cells to directly target the cancer once it’s put back into the patient.
Future of cancer treatment
Preliminary research from around the world indicates that immunotherapies for cancer are less toxic than conventional therapies like chemotherapy and radiation. They also have the potential for fewer and less severe side effects. This means that immunotherapies could improve patients’ quality of life.
Immunotherapies are effective, safe and relatively easy to manufacture. But they aren’t a standalone wonder drug that can bring about the end of cancer.
A multi-pronged approach that involves a combination of the best treatment options has been heralded as the next wave of therapeutic strategies for cancer and may provide a curative treatment.
Neelakshi Mungra, PhD Candidate at the MB&I Unit; Krupa Naran, Postdoctoral Research Fellow, Institute of Infectious Diseases and Molecular Medicine, University of Cape Town, and Trishana Nundalall, PhD Candidate at the MB&I Unit. The Medical Biotechnology and Immunotherapy Unit (MB&I) is an accredited research group at the University of Cape Town.









