Problem of antibiotic resistance under unprecedented scrutiny by new unit
03 July 2018 | Story Penny Haw. Photo supplied. Read time 9 min.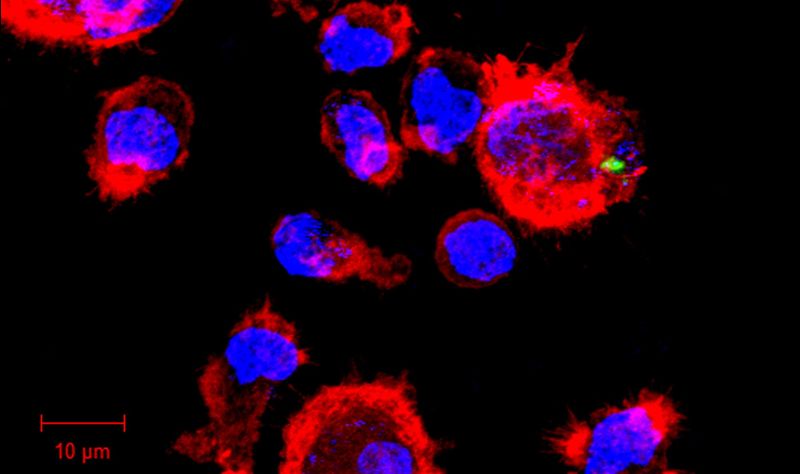
Funded by the South African Medical Research Council (SAMRC) and directed by UCT Professor of Respiratory Medicine, Professor Keertan Dheda, the recently established Centre for the Study of Antimicrobial Resistance (CAMRA) at UCT is an extraordinary development in the internationally urgent study of antimicrobial resistance among multidrug-resistant pathogens.
Not only will the work of the SAMRC Extra Mural Unit fortify the World Health Organisation’s (WHO) critical call for attention to the crisis of drug resistance – which has been prioritised alongside global warming – but it is also the first South African unit dedicated to studying the origin, development and fundamental drivers of antimicrobial resistance and multidrug-resistant pathogens.
“If the issues of antimicrobial resistance and multidrug-resistant pathogens are not addressed, we will head into a post-antibiotic era analogous to the 18th and 19th centuries. Common infections and minor injuries will once again kill people on a large scale,” says Dheda, who was last year awarded an A-rating by the National Research Foundation for his contributions to the field of pulmonology, with a specific focus on tuberculosis (TB). “This is already starting to happen.”
“Substantial morbidity and mortality due to multidrug-resistant infections, major health cost implications, and wider impact on society and the economy will not only retard economic growth, but there are also serious risks that it will undo the gains made under the United Nations’ Millennium Development Goals.”
The new centre will combine the efforts of several multi-disciplinary national and international authorities in the fields of TB and antimicrobial resistance to study the movement and distribution of drugs in the body, molecular sequencing and the development of inhaled drugs. The unit includes members and collaborators from the University of KwaZulu-Natal, University of Pretoria, Stellenbosch University, Walter Sisulu University, Sefako Makgatho Health Sciences University, SA National Institute of Communicable Diseases, London School of Hygiene and Tropical Medicine, University of Parma (Italy), and the Baylor Scott & White Research Institute in Dallas, Texas, in addition to those from UCT.
Given the high rate of drug-resistant TB in South Africa and because TB is a poverty- and HIV-related disease, Dheda says the unit will place special emphasis on this area of antimicrobial resistance. TB is now the foremost infectious disease killer worldwide and the commonest cause of death in South Africa. Almost 25% of TB strains globally are resistant to at least one major TB drug and drug resistant-TB contributes heavily to TB mortality.
“TB drug resistance and resistance to antibiotics threatens the gains we have made in health in South Africa,” says President of the SAMRC Professor Glenda Gray. “Bold efforts are required to tackle drug resistance at a global level and the SAMRC is committed to funding research that will endevour to find solutions that make global impact.”
Preventative strategies, antibiotics, vaccination, economic and psychosocial issues, and promotion of the appropriate use of antibiotics – also known as antibiotic stewardship – are among the many aspects of antimicrobial resistance that demand attention.
“A further worrying phenomenon is that there are hardly any new antibiotics entering the commercial pipeline,” says Dheda. “It is thus critical that newer and novel antibiotic classes be protected at all costs.
“However, this will not happen unless we understand the key drivers and pathogenesis of antibiotic resistance.”
We know that exposing bacteria to levels of antibiotic below what’s required to be effective is a key driver of antibiotic resistance. What is not known, however, is to what extent this occurs in specific clinical contexts, how resistance evolves and how it will be possible to prevent or at least minimise the development and evolution of resistance using better strategies for dosage and administration.
“CAMRA will address these key gaps in our knowledge,” says Dheda. “Moreover, we take a strategic view that inhaled antibiotics that supplement the primary treatment regimen will play an important role in antibiotic stewardship and effective treatment for multidrug-resistant pathogens. Thus, one of the long-term aims of the proposal is to establish a multi-disciplinary platform for the future study of inhaled antibiotics.
“This will address a further gap in current capacity and infrastructure as no such facility exists within South Africa.”
Vice president of research for the SAMRC, Professor Jeffrey Mphahlele elaborates, “The proposed work on AMR funded by the SAMRC is noteworthy in that it will also study non-TB AMR, which is a burgeoning health problem in South Africa.”
The unit’s initial objectives, says Dheda, can be categorised under three broad descriptions. CAMRA will:
- interrogate the relationship between drug concentrations and efficacy at the site of disease, including the lung;
- develop new methods to improve diagnostic sensitivity for the detection of rare populations of more resistant microbes undetectable by conventional methods in sputum and blood, and compare these to the site of disease; and
- conduct preliminary studies to determine the levels and efficacy of additional inhaled antibiotics at the site of disease both for TB and multidrug-resistant bacterial pneumonia. Thus, CAMRA will study both TB and non-TB bacterial pathogens.
“There are also important capacity development aspects of the project, including uplifting nascent academic centres, and championing transformation and gender equality,” explains Dheda.
The project is expected to span 10 to 15 years with the SAMRC funding addressing aspects of the team’s initial aims and helping to generate preliminary data to leverage further funding.
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.