A quiet (r)evolution: reimagining the undergraduate anaesthesia curriculum during a pandemic
09 December 2020 | Story Adalbert Ernst. Read time 4 min.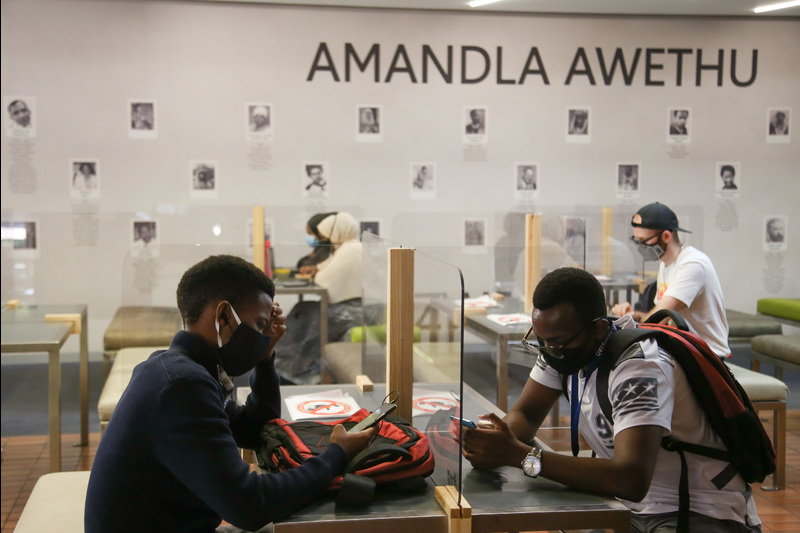
Dr Adalbert Ernst, Specialist and Undergraduate Convener for Anaesthesia in the Department of Anaesthesia and Perioperative Medicine reflects on his online teaching experience.
How do you teach one of the most practical specialties in medicine online to students who have never been in an operating theatre before? How will they graduate with the skill sets required to be safe and competent clinicians, when gaining practical experience is just too risky for all concerned? And how do you ensure that students remain awake so their future patients will be safely asleep?

One way is to have a small existential crisis about your dual role as clinician and teacher and think so far out of the box that you end up forgetting where the box was in the first place. With the shift to emergency online remote teaching, our Department’s undergraduate conveners had to create approachable learning content in brand-new formats in record time. While this was the lived experience for conveners in all undergraduate disciplines, anaesthesia faced additional pressures as the seemingly complete uncoupling of practical and theoretical training was magnified by the reality of a significantly-reduced clinical platform when students returned, unique staffing pressures, and the sobering fact that teaching the core skills of anaesthesia was (and currently still is) simply too risky for both students, patients, and clinicians alike.
As my fellow convener and I pondered all this, we knew we had to pull a sleight of hand involving reimagining everything we thought we knew about our courses, while trying to avoid reinventing several wheels. It was messy at first—very messy—interrogating the existing curriculum, and making hard decisions about what could be pruned, what could be grafted, and what could be done away with altogether.
The result was a leaner, streamlined, and updated organisation of our curriculum, mapped for the first time entirely around a patient’s perioperative journey. The foundational fourth year course was distilled online in modular format; the sixth year course was similarly structured around real-life clinical scenarios.
Answers and sanity often came from unexpected sources—those that lie so often in plain sight. I pondered the absurdity of 2020 and ultimately embraced it, inserting as much levity into our streamlined content as possible. My house became an impromptu film and recording studio. My wife, a clinician and educationist in a separate discipline, collaborated with me and we ended up creating content for each others’ disciplines, resulting in what one student called “a crossover that not even Marvel could have pulled off”.
As the clinical platform opened up and students returned, I networked with old friends and colleagues and tasked them to design a simulation course with the sophisticated equipment our Department already owns. Here the perioperative journey could be safely and holistically modelled for learners. These tutors also staffed dedicated workshops where the fundamentals of airway skills training are taught in a focused and systemic way.
“My house became an impromptu film and recording studio. My wife, a clinician and educationist in a separate discipline, collaborated with me and we ended up creating content for each other’s disciplines, resulting in what one student called ‘a crossover that not even Marvel could have pulled off'".
Some things have been difficult and sobering: shrinking skills logbooks to the bare and workable minimum, the loss of face-to-face teaching which I enjoy, and witnessing the strain on my full-time clinical colleagues.
There have also been unexpected joys: overwhelmingly positive feedback from students, the flexing of teaching muscles we never knew existed, and—most importantly for me as a convener—witnessing the retention (and improvement) of students’ learning. I also grew as a clinician and trudged home from busy calls appropriately weary, but sensing that I was emerging more focused and resilient in my day-to-day practice.
None of this would have been possible without the stellar support of my colleagues whose generosity of spirit continues to humble me.
I have come to learn that systems of knowledge are languages, and like all languages, they are living entities—as such, order often emerges out of chaos. Our courses have essentially evolved into new species fit for a new environment, and, for now, they are not just surviving, but even thriving.
Adalbert Ernst is a Specialist and Undergraduate Convener in Anaesthesia in the Department of Anaesthesia and Perioperative Medicine, Groote Schuur Hospital.
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.










