Mental health care can be cost-effective in poorer countries
13 April 2016 | Story Maggie Marx. Photo Michael Hammond.
On 13 April UCT's Programme for Improving Mental Health Care (PRIME) presented findings to world financial leaders in Washington which show that it's possible to narrow the large treatment gap for mental health care in low- and middle-income countries. The findings were presented at the World Bank and International Monetary Fund Spring Meeting.
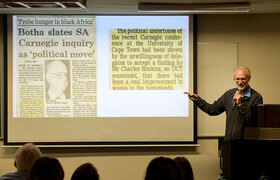
PRIME's Professor Crick Lund (lead investigator) presented recommendations for setting up, costing and evaluating mental health care plans in low- and middle-income countries. PRIME was selected out of a long list of mental health programmes worldwide to present at this inaugural event.
PRIME's goal is to generate evidence on the implementation and scaling up of treatment programmes for priority mental conditions in primary and maternal health care contexts in low-resource settings. The group is currently conducting research in South Africa, India, Nepal, Ethiopia and Uganda.
Their research has demonstrated that implementing mental health care plans is extremely cost-efficient. The PRIME team calculated the cost of implementing mental health care plans over a five- to 15-year scale-up period. These costs range from US$0.20 to 0.60 per capita in India, Nepal, Uganda and Ethiopia, and are close to US$2 per capita in South Africa.
“There is an urgent global need to address mental health as a public health and development issue,” said Lund, professor at the Centre for Public Mental Health. “Through our work in PRIME, we have developed processes and tools for ministries of health, NGOs and other researchers to implement and scale up mental health services in other low- and middle-income countries.”
The unmet need for mental health care is high in most low- and middle-income countries. The consequences of untreated mental disorders include suffering, diminished quality of life, disability, human rights abuses, stigma and discrimination, poverty, poor physical health and premature mortality.
The next stage of PRIME research will include evaluation of the implementation of the mental health care plans as well as further research on scaling up the programme.
For more information or to request interviews, contact PRIME at maggie.marx@uct.ac.za or visit the PRIME website.
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.