Nurses given tools to fight TB
10 October 2005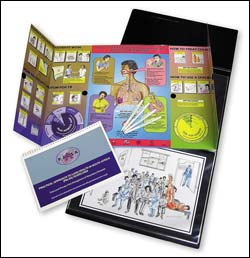
Nurses, at the front line of health care in South Africa, are learning to diagnose patients with life-threatening illnesses such as tuberculosis. A pilot training programme in the Free State done in collaboration with the UCT Lung Institute, has shown real results and is about to be extended to the Western Cape.
The World Health Organisation (WHO) estimates that most people who develop tuberculosis are never diagnosed, and so don't benefit from treatment. In South Africa, detection of tuberculosis remains a significant challenge to the health service, particularly in the light of the HIV and AIDS pandemic.
Respiratory diseases share common symptoms, like coughing and difficult breathing, and sufferers usually seek help from health workers in primary care. For most South Africans using the public sector, this task falls to nurses. These nurses are responsible for distinguishing serious conditions, like tuberculosis, from the usual colds and flu.
Now a new training intervention for South African nurses is giving them the tools to improve the quality of care for respiratory patients, including diagnosing tuberculosis.
A trial, published last week in the British Medical Journal, found that the pilot training programme in the Free State, called Practical Approach to Lung Health in South Africa (PALSA), substantially improved the quality of care for respiratory patients, including increased detection of tuberculosis cases, and improved asthma management.
PALSA was developed by UCT's Lung Institute, in collaboration with the Medical Research Council (MRC), the Universities of the Free State, Western Cape, Toronto and East Anglia.
PALSA is a set of evidence-based guidelines that use symptoms to guide nurses to the correct diagnosis and treatment. After all, most people attending primary care present with symptoms and not a diagnosis.
These guidelines are combined with knowledge-translation strategies that include a variety of specialised education approaches and aids used to keep health professionals up to speed with the latest developments and treatments.
These strategies are used extensively in the US and Europe to ensure that doctors prescribe the most effective medication and treatments for their patients.
As part of an educational outreach approach, nurse trainers visit primary clinics and deliver short, focused interactive training, with the help of the guidelines and illustrated support materials.
PALSA was developed and tested among primary-care nurses in the Free State during 2003, leading to tangible improvements in care and diagnosis. The intervention also proved extremely popular with nurses, and has since been expanded to cover HIV and AIDS, at the request of the Free State Department of Health. The expanded guidelines are now being widely used in the province's antiretroviral treatment services.
The Western Cape Department of Health is also planning to roll out the PALSA intervention in its primary-care clinics with a view to improving tuberculosis detection. The project highlights the important role researchers can play in designing relevant and effective interventions to address priority diseases in South Africa.
The British Medical Journal launched its special theme issue on Africa - focusing on topics ranging from HIV/AIDS to malaria, heart disease and diabetes - at UCT on September 29. The edition was guest-edited by Professor Jimmy Volmink, chair of primary health care at UCT. Associate editor Jocalyn Clark, who flew in to Cape Town for the occasion, said: "We hope this theme issue encourages greater dialogue and collaboration between doctors and researchers in the North and the South. It's a call to see the promise and potential of Africa, not just the struggle and suffering."
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.










