Long-term neuropsychological outcomes in severe COVID-19
06 December 2021 | Story Supplied. Photo Getty Images. Read time 6 min.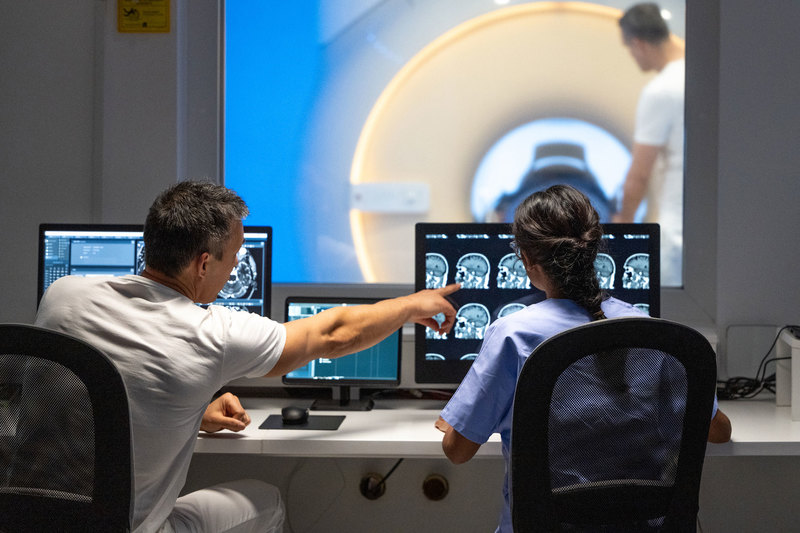
In collaboration with Professor Mark Solms, who is the chair of neuropsychology at the Neuroscience Institute, University of Cape Town (UCT) alumnus Dr Donné Minné hopes to document cognitive and neuropsychiatric repercussions in a study funded by the National Research Foundation.
People who develop severe illness from COVID-19 have a much higher risk of neurological and mood-related disorders, particularly if they have been hospitalised. These effects have been linked to several pathological events in the body, including systemic inflammation, blood vessel changes, alterations in the blood–brain barrier, loss of oxygen to the brain and the consequences of mechanical ventilation. As a result, many patients suffer lasting difficulties with memory, concentration, low motivation, and anxiety.
“These symptoms pose a major challenge to independent living and general well-being, and are likely to heavily impact mental health,” said Dr Minné, who is a postdoctoral fellow and neuropsychologist who trained through UCT’s Department of Psychology.
Neurological ailments
Since early in the pandemic, neurological ailments have been observed and documented in a large proportion of critically ill COVID-19 patients; they include impaired consciousness, seizure, stroke and motor-neuron dysfunction, among others. Studies on neuropsychological outcomes (a branch of psychology that deals with how mental functions such as thoughts and feelings relate to specific brain correlates) have only come to light more recently. These show that severe infection with SARS-CoV-2 can lead to persisting deficits in memory, attention and executive functioning, and declines in the general speed at which an individual can process information.
Appropriate care – especially psychosocial support, to address the trauma and loss associated with brain injury – is a key part of the rehabilitation process.”
“Patients presenting with these symptoms might experience forgetfulness, difficulties with concentration, and trouble following conversations or finding the right words. This can feel disorienting and overwhelming. One consequence is that people tend to experience anxiety and might prefer to self-isolate. Fatigue is also very common in COVID-19 ICU survivors and can be debilitating. Appropriate care – especially psychosocial support, to address the trauma and loss associated with brain injury – is a key part of the rehabilitation process.”
Research undertaken prior to the COVID-19 pandemic shows that up to 40% of patients who require mechanical ventilation suffer cognitive impairment in the long term, and we should therefore expect similar outcomes in COVID-19 patients who develop acute respiratory distress syndrome. However, SARS-CoV-2 can also disrupt central nervous system functioning in patients who do not develop acute respiratory distress, suggesting multiple pathways of damage.
Studies and findings
In some older patients, evidence is emerging that a severe course of COVID-19 may exacerbate or even trigger progression to some forms of dementia. Risk factors for dementia, such as age, hypertension, diabetes and cardiovascular disease are also major predictors of COVID-19 severity. One common denominator in these risk profiles is inflammation. In fact, one of the major shifts in Alzheimer’s Disease research over the past decade has been a spotlight on the role of inflammation and dysregulation in immune-related pathways, as central events in the pathological cascade of neurodegeneration.
A study undertaken in the United Kingdom and published in the Journals of Gerontology showed that carriers of the ε4 allele of the APOE gene, which has been linked to Alzheimer’s Disease risk, were twice as likely to require hospitalisation for COVID-19 illness than people who were carriers of the more common APOE ε3 genotype. The APOE gene is mainly involved in the synthesis and storage of lipids; however, studies have shown it to be critical for biological processes linked to neuroprotection, such as the regulation of oxidative stress and inflammation. APOE ε4 is associated with increased inflammatory cytokine response. This suggests that carriers are more vulnerable to becoming critically ill from COVID-19, and this disease course might compound risk for dementia in the long term.
It is … important that studies include patients from different backgrounds, and assess cognition and mood much further down the line.”
While these findings are cause for concern, we should not be jumping to conclusions.
“There are still many unknowns regarding the nature and trajectory of neuropsychological outcomes following COVID‐19 infection. Most of the currently available knowledge comes from data collected from patients in Europe and the United States, during the very early phases in a person’s recovery. Yet recovery from brain injury can take up to two years, and is influenced by a number of individual factors, such as age, education and social support. It is therefore important that studies include patients from different backgrounds, and assess cognition and mood much further down the line.”
This collaborative study between Cape Peninsula University of Technology and UCT is taking place at the Neuroscience Institute at Groote Schuur Hospital in Observatory, Cape Town. All members of the public who have been hospitalised for COVID-19 are invited to take part. Participation will involve a two-hour visit to the Neuroscience Institute, during which time participants will undergo assessments of cognitive skills, such as memory and concentration, and be asked to share information relating to mood and emotions. All participants will receive reimbursement for travel costs and be entitled to a debriefing session to receive feedback on their results. To participate, please send an email to covidandthebrain@gmail.com.
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.
Research & innovation















-Landscape.jpg)





















