UCT sickle cell genetics study a first for Africa
25 August 2020 | Story Nadia Krige. Image Keith Chambers, Wikimedia. Read time 10 min.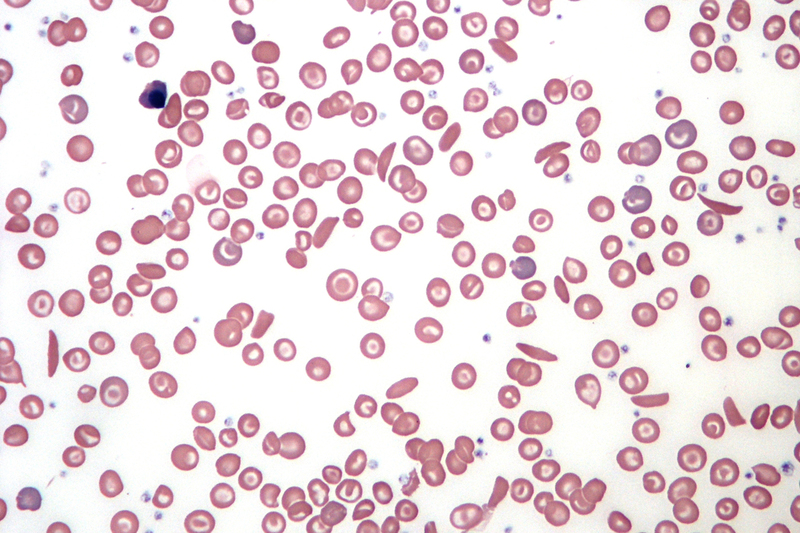
New research investigating the genetic modifiers of long-term survival in individuals with sickle cell anaemia (SCA) reveals a range of possible pathways for novel therapeutic interventions. Professor Ambroise Wonkam, principal investigator and director of Genetic Medicine of African Populations (GeneMAP) in the University of Cape Town’s (UCT) Division of Human Genetics, says apart from the study’s clinical potential, the fact that it is so deeply rooted in Africa also presents the opportunity for a paradigm shift in science policy and diplomacy.
Sickle cell disease (SCD) is the umbrella term for a range of inherited disorders in which the red blood cells have an abnormal crescent or banana shape, which block small blood vessels. As a monogenic disorder, it is caused by a mutation in a single gene, which is responsible for production of the protein, haemoglobin. Making up 70% of the content of red blood cells, haemoglobin is essential for the transportation of oxygen through the body. SCA is the most severe manifestation of SCD and, therefore, the focus of Wonkam’s study.
“Among the 300 000 babies that are born with the condition every year, 80% are in sub-Saharan Africa.”
What makes SCA particularly interesting as a genetic disorder, is its prevalence in sub-Saharan Africa.
“Among the 300 000 babies that are born with the condition every year, 80% are in sub-Saharan Africa,” says Wonkam. “It is, in essence, an African disease.”
Counterintuitively, however, over the past 50 years, most of the truly critical research into SCA has been conducted outside of Africa – mostly in Europe and the United States.
With its cohort of 192 African SCA patients recruited at African hospitals and conducted at an African university by African researchers, Wonkam’s genetic study, using next generation DNA sequencing, is truly a first for the continent.
The curious case of long survivors
Despite the prevalence of SCA in Africa, medical care has been less than optimal. This can be ascribed to several factors, including lack of access to resources and non-availability of specific effective interventions, such as the screening of newborn infants and systematic penicillin use for the presentation of infections.
According to Wonkam, it has been shown that, due to this lack of clinical interventions, in most African settings, at least 50% of African children with SCA will die before they turn five years old.
Simultaneously, however, the same regions of sub-Saharan Africa are also home to SCA patients who have turned 50 or 60 years old.
“Why is it that these people - who live in an environment that is not favourable in terms of healthcare access, and stressors including high temperatures, malaria and other infections – manage to survive while others die at a much younger age?” Wonkam asks. “Our hypothesis is that these long survivors living with SCA may be protected by some genetic factors.”
In most African settings, at least 50% of African children with SCA will die before they turn five years old.
Furthermore, he explains, if this is indeed the case, the genetic modifiers present in these individuals may hold the key for exploring new routes of treatment for other SCA patients. “If we know how it works in their body,” he says, “we can provide new treatment looking at those pathways.”.
Whole exome sequencing
Comparing the human genome to a library, and the 20 000 genes it contains to books, Wonkam explains:
“We wanted to understand by looking at all the 20 000 books – the 20 000 genes that they have – and see if we can find a signature that may have allowed them to survive longer.”
In scientific terms, this process is known as whole exome sequencing and is performed by extracting DNA from the white blood cells contained in a patient’s blood. The DNA is then stretched, and its contents ‘read’ by a machine called the ‘whole exome sequencer’. The patient’s exome is then aligned to reference exomes for comparison to pick up on any deviations.
Recruiting a study cohort
Of course, the most crucial aspect of a study of this nature is recruiting a feasible cohort of patients.
Wonkam and his research team started by recruiting SCA patients of 40 years or older who had received minimal clinical interventions. They then selected a control group of patients who had suffered from strokes, one of the most severe effects of SCA, as well as an ‘intermediate’ group who were under 40 and had never experienced a stroke.
The recruitment process took place in Cameroon and produced a study cohort of 25 long-survivors, 25 stroke patients and 50 intermediate patients.
To ensure that the study’s outcomes were valid beyond the Cameroonian cohort, the researchers recruited a replication cohort in Cape Town, which consisted mostly of patients from the Democratic Republic of Congo.
Illuminating possible new treatment pathways
As Wonkam had suspected, the study revealed that patients in the long-survivor group did indeed present certain genetic modifiers that patients in the stroke group did not.
In the long-survivor group, enriched genes included CLCN6, for which rare deleterious variants have been associated with lower blood pressure and OGHDL, which is important in the metabolism of the amino acids arginine and glutamine.
“We found that people who had survived longer, had recurrent changes in those genes,” explains Wonkam.
He goes on to say that one of the most interesting aspects of this finding, was the fact that glutamine was recently validated as a treatment for SCA by the Food and Drug Administration (FDA), in the United States of America (USA).
“I believe this is probably one of the landmark findings that have been performed in Africa where most of these patients live.”
“This means that some of the patients actually make glutamine available to themselves naturally,” Wonkam says. “In other words, they are naturally able to treat themselves.”
Other interesting findings in the long-survivor group included more efficient metabolism of the micronutrient selenium as well as the presence of genes that assist in keeping blood pressure low.
In the stroke cohort, the researchers found that patients tended to have a mutation in the blood coagulation pathway. Wonkam says this implies that thinning the blood of SCA patients may be a clinical intervention worth investigating.
“What our study has shown is that there could be a few other routes for therapeutic manipulation that have not yet been explored,” he says.
For a disease where the current definitive treatment is a bone marrow transplant, and – in the near future - gene therapy and gene editing, this provides a major breakthrough.
“At the moment, we do not yet have widely available treatment that is affordable to the 300 000 babies born with sickle cell disease every single year worldwide.”
Breaking new ground for Africa
Something that Wonkam says is critically important about this study, is the fact that for the last 50 years most of the truly critical research into SCD took place in Europe and America.
“I believe this is probably one of the landmark findings that have been performed in Africa where most of these patients live,” he says.
“It is our hope that this may shift a bit of paradigm in terms of science policy and diplomacy. We hope that funders will see what can actually be done in Africa and channel more means here. We also hope that this will help amplify the voices of more researchers that are working on SCD in Africa.”
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.










