How a gene test can solve side effects linked to ARV drugs in Africa
29 January 2017 | Story Collen Masimirembwa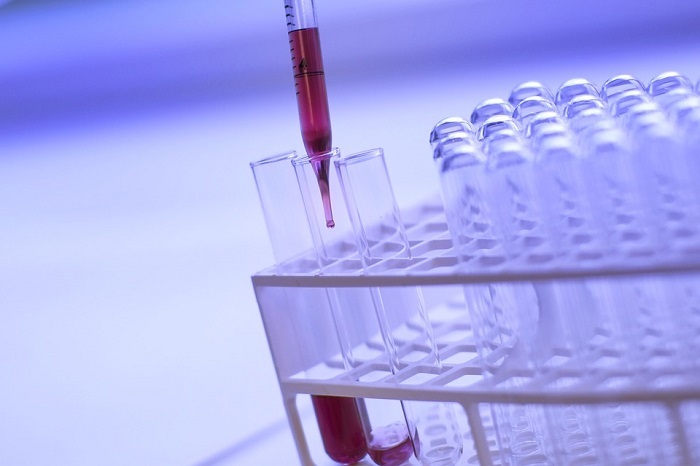
Antiretrovirals have significantly improved the lives of people living with HIV. Today there are more than 17 million people on treatment and the number of deaths from the disease has been drastically reduced.
But many people who take the treatment regimens daily experience severe side effects. Adverse drug reactions result in people not sticking to the treatment regime. This in turn leads to poor treatment outcomes and the risk of resistance developing.
One particular antiretroviral – efavirenz – presents a challenge.
It is considered one of the most cost effective antiretroviral treatments available and is recommended by the World Health Organisation (WHO) as a firstline treatment against HIV. By 2014 just less than half of all the people on antiretrovirals in low and middle income countries – that’s 8 million – were on the drug regime.
But up to 50% of patients taking it have to change treatment within a year. And the World Health Organisation has it on its list of drugs with the harshest side effects. People taking the drug can experience serious neuropsychiatric drug reactions including depression, nightmares, headaches and suicidal tendencies.
But there may be a solution.
Studies have shown that people who react particularly badly to efavirenz have a particular gene variant that messes with an enzyme responsible for processing the drug in their bodies.
We set out to find a way for patients to continue using the drug without the side effects. As part of our study we developed a mechanism to test whether people have this gene. Those that test positive for the genetic variant can be put on reduced doses of the drug. It remains effective but is less toxic.
This is an important step because it addresses three problems: it makes it possible for people to stick to continuous treatment cycles; this in turn reduces the risk of resistance developing; and it means that a cost effective antiretroviral treatment can be administered better.
At the current dose of 600 mg daily patients who have variations of a specific gene – CYP2B6 – have a higher chance of developing side effects because of toxic blood levels. We did a continent wide population genotyping study with 11 major African populations groups to establish how prevalent this genetic variant was.
The population groups were the Yoruba, Ibo, Hausa tribes in Nigeria, the Kikuyu, Luo, Masaai in Kenya, mixed groups of Tanzania, the Venda in South Africa and the Shona, Ndebele and San in Zimbabwe.
We found there was a 30% to 60% likelihood of the genetic variant being found in African populations. This is compared to a 15% to 20% likelihood in white and Asian people.
Using this information we were able to derive a dosing algorithm that could be used to tailor drug doses in patients with the gene variant.
The algorithm indicates that patients who have two low activity variants should be given 200 mg of the drug instead of the standard 600 mg. Those who have one normal activity and one low activity variant should be given 400 mg per day.
Our studies were done in our laboratory in Zimbabwe and then replicated in South Africa, Tanzania, Uganda and Ethiopia by independent research groups.
This algorithm is now being developed into a test kit – GeneDose-EFV test kit – which can be used in clinics.
It is not the first time that antiretrovirals have caused serious side effects in patients. But it took up to five years to physically remove the drug with side effects due to the number of places that it had been distributed to across the continent.
The widespread use of efavirenz on the continent, and the fact that it’s inexpensive, means there is an urgent need to address the burden of its adverse effects without dropping it as a treatment option.
There are several benefits from the test. Patients can stay on the drug by being given a dose they can tolerate. This, in turn, will result in increased treatment compliance among patients and therefore less of a risk for HIV drug resistance.
And for governments, it means they will still be able to administer cost effective antiretroviral treatment at a public health level and keep more patients on sustained antiretroviral treatment at a cheaper cost.
Collen Masimirembwa, Honorary Prof. of Clinical Pharmacology,, University of Cape Town.
But many people who take the treatment regimens daily experience severe side effects. Adverse drug reactions result in people not sticking to the treatment regime. This in turn leads to poor treatment outcomes and the risk of resistance developing.
One particular antiretroviral – efavirenz – presents a challenge.
It is considered one of the most cost effective antiretroviral treatments available and is recommended by the World Health Organisation (WHO) as a firstline treatment against HIV. By 2014 just less than half of all the people on antiretrovirals in low and middle income countries – that’s 8 million – were on the drug regime.
But up to 50% of patients taking it have to change treatment within a year. And the World Health Organisation has it on its list of drugs with the harshest side effects. People taking the drug can experience serious neuropsychiatric drug reactions including depression, nightmares, headaches and suicidal tendencies.
But there may be a solution.
Studies have shown that people who react particularly badly to efavirenz have a particular gene variant that messes with an enzyme responsible for processing the drug in their bodies.
We set out to find a way for patients to continue using the drug without the side effects. As part of our study we developed a mechanism to test whether people have this gene. Those that test positive for the genetic variant can be put on reduced doses of the drug. It remains effective but is less toxic.
This is an important step because it addresses three problems: it makes it possible for people to stick to continuous treatment cycles; this in turn reduces the risk of resistance developing; and it means that a cost effective antiretroviral treatment can be administered better.
Finding the problematic gene
At the current dose of 600 mg daily patients who have variations of a specific gene – CYP2B6 – have a higher chance of developing side effects because of toxic blood levels. We did a continent wide population genotyping study with 11 major African populations groups to establish how prevalent this genetic variant was.
The population groups were the Yoruba, Ibo, Hausa tribes in Nigeria, the Kikuyu, Luo, Masaai in Kenya, mixed groups of Tanzania, the Venda in South Africa and the Shona, Ndebele and San in Zimbabwe.
We found there was a 30% to 60% likelihood of the genetic variant being found in African populations. This is compared to a 15% to 20% likelihood in white and Asian people.
Using this information we were able to derive a dosing algorithm that could be used to tailor drug doses in patients with the gene variant.
The algorithm indicates that patients who have two low activity variants should be given 200 mg of the drug instead of the standard 600 mg. Those who have one normal activity and one low activity variant should be given 400 mg per day.
Our studies were done in our laboratory in Zimbabwe and then replicated in South Africa, Tanzania, Uganda and Ethiopia by independent research groups.
This algorithm is now being developed into a test kit – GeneDose-EFV test kit – which can be used in clinics.
A quicker and cheaper solution
It is not the first time that antiretrovirals have caused serious side effects in patients. But it took up to five years to physically remove the drug with side effects due to the number of places that it had been distributed to across the continent.
The widespread use of efavirenz on the continent, and the fact that it’s inexpensive, means there is an urgent need to address the burden of its adverse effects without dropping it as a treatment option.
There are several benefits from the test. Patients can stay on the drug by being given a dose they can tolerate. This, in turn, will result in increased treatment compliance among patients and therefore less of a risk for HIV drug resistance.
And for governments, it means they will still be able to administer cost effective antiretroviral treatment at a public health level and keep more patients on sustained antiretroviral treatment at a cheaper cost.
Collen Masimirembwa, Honorary Prof. of Clinical Pharmacology,, University of Cape Town.
This article first appeared in The Conversation, a collaboration between editors and academics to provide informed news analysis and commentary. Its content is free to read and republish under Creative Commons; media who would like to republish this article should do so directly from its appearance on The Conversation, using the button in the right-hand column of the webpage. UCT academics who would like to write for The Conversation should register with them; you are also welcome to find out more from carolyn.newton@uct.ac.za.
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.
Related
Why South Africa's carbon tax should stay
24 Feb 2026
Republished
Cape Town’s wildflowers: six key insights from a new checklist
19 Feb 2026
Republished