Your brain on drugs
18 August 2014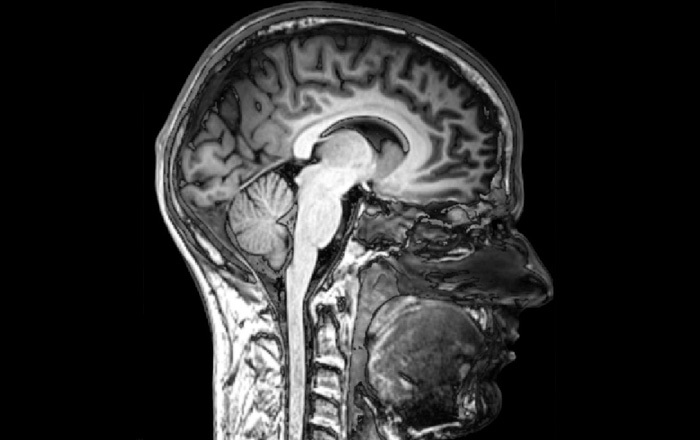
In what is considered one of the most memorable anti-narcotics advertisements in history, commissioned by the Partnership for a Drug-Free America, an egg is shown frying in a pan with a voiceover proclaiming, "This is your brain on drugs. Any questions?" Yet there are many complex questions that still need answering when it comes to the neuroscience of drug addiction.
What scientists have been able to determine in the past generation is that drug addiction is a neurological disease - a biologically complex, progressive, insidious illness that rewires the brain's chemistry, and ultimately, your behaviour. "Research shows how drugs hijack the brain and cause long-lasting changes in brain function that are difficult to reverse," explains Dr Volker Hitzeroth, a Cape Town psychiatrist and author of The End of Addiction. "It is really difficult to beat the disease of addiction - a truly biological-psychological-social disease - because your brain cells gang up on you. It's an unwanted condition, because nobody goes out to become an addict."
How the brain is hijacked
To understand the neurobiological mechanisms of addiction, you need to know that drugs affect the brain's reward pathway - as well as the brain's centres of planning, emotional processing and memory (the prefrontal cortex, amygdala and hippocampus respectively).
The reward pathway starts at a group of nerve cells at the very centre of the brain, the ventral tegmental area (VTA), that receives messages on how well the body's fundamental needs are being met, and then forwards these messages along to another cluster of nerve cells, the neucleus accumbens. It transmits this information using a chemical messenger, dopamine.
The most basic explanation of what this pleasure circuit does is that it makes you feel motivated and rewarded. "However, what dopamine in this system actually does is it gives salience," explains Hitzeroth. "When something causes dopamine surges, your brain attributes meaning [to it], and prioritises this something as important for survival."
Addictive drugs hijack this system by increasing the VTA's ability to flood the circuit with dopamine, effectively creating a shortcut to pleasure. "Nowadays, drugs cause a much higher and quicker dopaminergic surge because they've been highly refined through chemical processes," says Hitzeroth. "This is why they are so much more dependency-forming."
Through brain-imaging studies, we now know that drug abuse also causes dysfunctionality in the prefrontal cortex - the part of the brain that regulates your impulses and emotions, and is important for analysing, regulating, rationalising and flexibility. "All these vital functions become less controlled as a dependency is formed, and see an individual losing their willpower when it comes to abstaining from drugs," says Hitzeroth.
Drug abuse also affects the hippocampus (where memories are formed, modulated and stored) and the amygdala (where emotions are decoded). "These two bodies become responsible for storing the drug memories too: the emotional memories of the 'high', the temptation of drug abuse. And if you're unable to manage your memories, then you're more likely to be tempted to use drugs, because you only remember the 'high'," says Hitzeroth.
"Then add the additional influence of, for example, neurodevelopment, genetics, experience, peer pressure, social rules, whether you've been taught delayed gratification or not, and so on, and you've got a massively complex neurobiological system that has been hijacked by drug use over time, which then predisposes an individual to using drugs and relapsing."
The journey to addiction
A key research paper titled A Multistep General Theory of Transition to Addiction, by authors Pier Vincenzo Piazza and Véronique Deroche-Gamonet, published last year in the journal Psychopharmacology, provides a coherent theory on the latest thinking regarding neuroscience and addiction as a true psychiatric disease, says Hitzeroth.
"The major principles are, firstly, that the transition to addiction results from interactions between individual vulnerability and the degree or amount of drug exposure. Secondly, this transition involves a three-step sequential process, namely sporadic recreational use; then intensified, sustained, escalated use; and finally, loss of control."
More simply put, the first step towards addiction is when the centre of the brain's reward system, the nucleus accumbens, is flooded with dopamine, and the brain learns to associate drugs with pleasure. "Here, individuals learn to use drugs even if their first experience was awful.
"In the second step, there's a move from physiology to pathophysiology, so now there are changes made to the brain that are abnormal - the brain is being moulded."
This is particularly prevalent in individuals who have a hyperactive reward system or an impaired prefrontal cortex. "Here, sustained and prolonged drug use induces incentive sensitisation: the more drugs you take, the more your dopaminergic system revs up. This is the opposite of drug tolerance. At this stage, drugs become the new normal."
The final stage - loss of control - is only reached through long-term drug exposure. Your brain loses its synaptic plasticity: nerves become less flexible, and have trouble growing and making new connections. This in turn crystallises drug-taking behaviour, and you lose control of your urges and intake. At this point, drugs are not only wanted and needed, but also pathologically mourned when absent.
Healing the brain
If the neurological damage caused by drug addiction is so devastating, how long does the brain take to heal?
"The short answer is, nobody knows," says Hitzeroth. "Some research says one to three years, while other studies say four to ten years - and the AA says, 'Once an addict, always an addict.' Their thinking isn't faulty, as the brain has been hardwired differently.
"So how do you change the hardwiring of the brain? Very slowly - and with abstinence."
Fortunately, the success rate of treatment is good, Hitzeroth adds: "A research paper has compared the recovery outcomes for the chronic diseases of addiction, diabetes and high blood pressure - addiction isn't worse than the others in terms of success rates. But this is only if the addict gets good, evidence-based treatment - with the assistance of a doctor, psychologist and social worker - which there is a dire shortage of in South Africa."
 |
 |
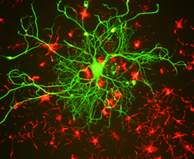 |
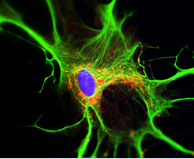
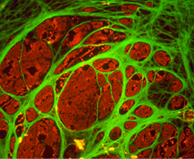
| A rat astrocyte (a star-like cell in the brain) growing in a Petri dish, courtesy of Drs Edward Nyatia and Dirk Lang, in collaboration with Damien Schumann and Brainstorm the City. • A cultured oligodendrocyte, which helps ensure fast and efficient electrical signalling of neurons, isolated from the spinal cord of a xenopus frog. Image courtesy of Dr Dirk Lang, in collaboration with Damien Schumann and Brainstorm the City. • Neuron in tissue culture by Gerry Shaw, licensed under Creative Commons Attribution-Share Alike 3.0 via Wikimedia Commons | ||
Story by Carla Calitz.
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.










