Adolescent nephrology clinic plugs ‘critical gap’ between paediatric and adult care
01 March 2024 | Story Niémah Davids. Voice Cwenga Koyana. Read time 9 min.
For more than two decades, a clinic dedicated to caring for adolescents and young adults with advanced kidney disease has made its mark – thriving in the heart of Groote Schuur Hospital (GSH), as it serves patients across Cape Town in need of specialised care.
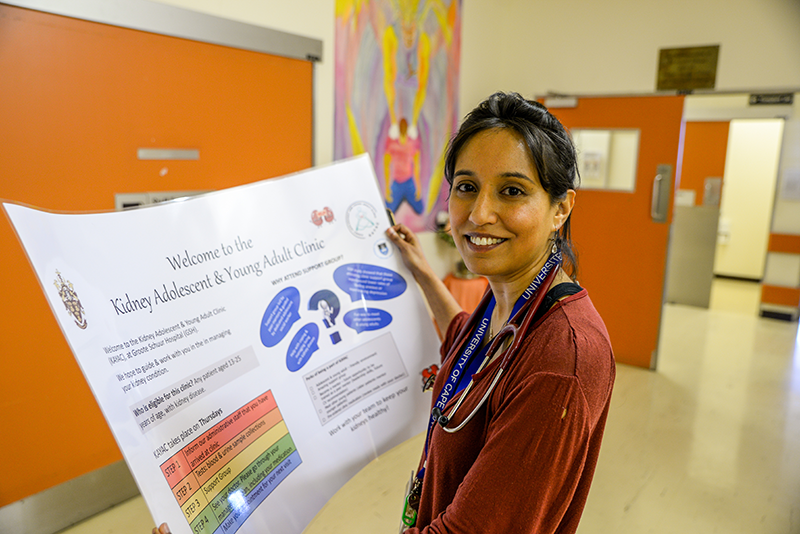
The Kidney Adolescent and Young Adult Clinic (KAYAC) was established to plug a critical gap between paediatric and adolescent care and to ensure patients with chronic kidney disease are adequately supported as they learn to navigate their new normal outside the paediatric healthcare setting. KAYAC is the only one of its kind on the continent. It was founded in 2002 and redesigned in 2015 under the auspices of the University of Cape Town’s (UCT) Professor Mignon McCulloch and Dr Bianca Davidson. Today, KAYAC is headed by UCT’s Dr Zibya Barday in partnership with a multidisciplinary team, including an adult and paediatric nephrologist, a nurse practitioner and social worker. The clinic has evolved into one of the leading kidney transition clinics in Africa.

Since KAYAC first opened its doors, Keenan Solomon and Tarique Kenny are two out of thousands of patients who have benefited from the clinic. Solomon’s and Kenny’s friendship blossomed as toddlers in the Nephrology Unit at the Red Cross War Memorial Children’s Hospital. At the time, both needed a kidney transplant and spent extended periods of time in hospital. A few years ago, the duo transitioned to GSH’s KAYAC, marking a significant step in their health, well-being and friendship.
“KAYAC has been a very big part of my life since I made the transition from Red Cross five years ago. It’s where I received my dad’s kidney with a transplant in 2019. And for me, it’s a safe space. It’s a space where we come together and learn about the importance of taking good care of ourselves, especially for those of us with chronic conditions. But it’s also a space where we can connect and just be because we understand each other,” Solomon said.
Transition care model
According to Dr Barday, the clinic was designed to help patients make a smooth transition from paediatric to adult care, and the need, she added, is not just unique to South Africa. Sadly, one too many times patients with kidney disease fell through the cracks because the switch from paediatrics to adult care, and from one health facility to another, was not seamless. And while the transition phase is important for all young nephrology patients, for kidney transplant recipients like Solomon and Kenny, it is “absolutely critical”. These patients require specialised care and support and can’t afford to miss a single clinic visit or stop their medication.
“We acknowledge that the move can be daunting, and due to a lack of support, patients may not be as diligent with their follow-ups as before. This can be very dangerous, because non-adherence to medication could lead to kidney disease progression, and even kidney allograft rejection,” she said. “So, what we have done is introduce a transition system that encompasses a purposeful and planned movement of adolescents with chronic kidney illnesses from paediatric to adult care, and the clinic has grown from strength to strength.”
Barday and her team work closely with the Red Cross War Memorial Children’s Hospital’s Nephrology Unit. And through KAYAC’s transition care model, clinicians regularly engage with patients who are preparing to exit the paediatric phase. KAYAC prepares patients for the shift from a parent-centred, fully supervised care, to a more self-sufficient, autonomous role. She said family members are central to these discussions to maintain the family-centric approach nurtured in paediatric care. The clinic provides an “adolescent-young, adult-friendly” environment, with evidence-based best practice kidney care tailored for each individual. And the model continues to serve its purpose. Barday said a recent research study revealed that patients who attend the clinic recorded better kidney outcomes because they remain committed to their follow-up sessions and lower mortality rates, when compared to young adult patients who attend the traditional adult kidney service.
Interactive, stimulating, nurturing environment
Once patients have made the transition, their number of clinic visits depend on their conditions. Barday said some patients are required to visit the clinic regularly, while others visit once a month or once every second month. Their sessions include time with the resident nephrologist and clinic nurse and comprise a full clinical exam to ensure they’re on the right track, have remained “engaged in their well-being” and adherent to their medication. The clinical session also offers the patient the opportunity to discuss any concerns with a trained clinician.
But clinic visits are not just for serious business. And for Solomon, who also serves as a patient mentor, his visits are the highlight of his month. Before the clinical exam, patients unwind and connect with each other during a support group session. They play board games, listen to music or participate in a drama or karate class. He said the young adults are also taught valuable life skills, as well as interpersonal and conflict resolution skills, and engage in discussions and debates on important events affecting the world.
“We get to laugh and relax, but at the same time we don’t lose sight of the reason that we are here.”
“These social slots are the flip side of the coin. We get to laugh and relax, but at the same time we don’t lose sight of the real reason that we are there. The road was not easy – not for any of us or our families. I know my parents, Ashley and Ruth, and my extended family made many sacrifices for me. It’s been a very hard road. But this is the second chance we prayed for, and we need to make sure we keep healthy. This clinic allows us to do this, and I thank everyone involved for this opportunity,” Solomon said.
Seeing the world through a different lens
And Kenny feels the same. He said the clinic has played an instrumental role in his post-transplant journey and has helped him see the world through a different lens. Thanks to staff members’ constant encouragement, he has managed to accept his chronic kidney condition – cystinosis – a rare genetic disorder that typically affects the kidneys and causes an amino acid to build up in the body’s cells. This process leads to crystallisation, which in turn affects the organ’s functionality.
“Being here has meant so much. In the beginning, I must admit, I was fearful. It was an unknown environment and very different to Red Cross. But I reminded myself that I’m here for a reason and I needed to make the best of it, and I adjusted quickly. The clinic gave me that independence I needed,” he said.
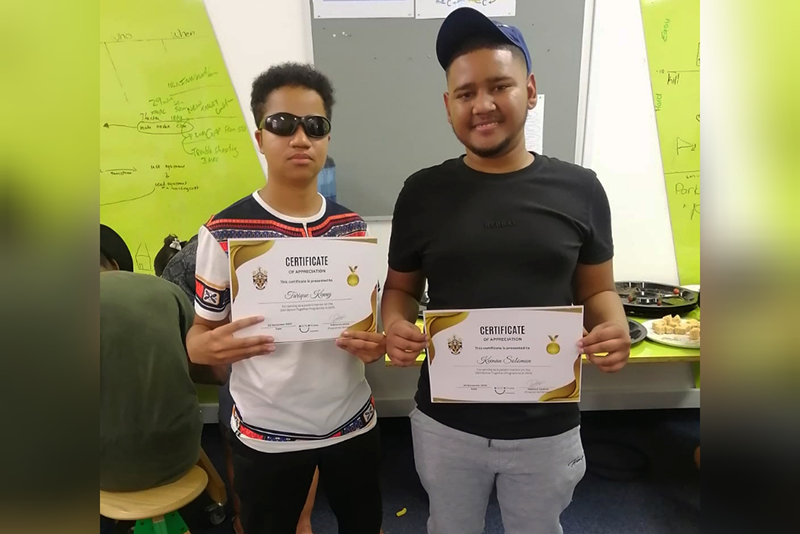
Because few people realise that dealing with a chronic condition becomes increasingly difficult as the patient moves into adulthood, Kenny said a solid support system other than immediate family and friends is important. And KAYAC provides that. Like Solomon, he considers it a safe space and a platform to connect with likeminded young adults whose struggles are similar to his.
‘I’m a better person because of it’
Kenny, an aspiring actor, who’s made his debut on local telenovela Arends Vlei, has enjoyed serving fellow patients in a mentorship capacity, getting to know them on a different level, and understanding their challenges.
“People open up during our sharing sessions and some stories break the heart. Some I can relate to, others not. And so, being a mentor has taught me a different level of compassion. It’s taught me to listen to understand and not just for the sake of listening. It’s taught me to have empathy and to remember that our contexts play such a big role in who we are. It’s safe to say that the clinic continues to conscientise me on all of this and I’m a better person because of it,” he said.
Over the years, Solomon and Kenny have learned to embrace their chronic kidney conditions, as well as the long list of things that go with it, including their regular clinic visits, their daily doses of medication and maintaining a healthy, well-balanced lifestyle. What matters now is “living our lives to the full” and encouraging those patients out there with similar stories to do the same.
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.
Faculty of Health Science News
























