Tackling TB one breath at a time
15 March 2019 | Story Laura Rawden. Photo Janice Haney Carr, Dr Ray Butler, Pixnio. Read time 7 min.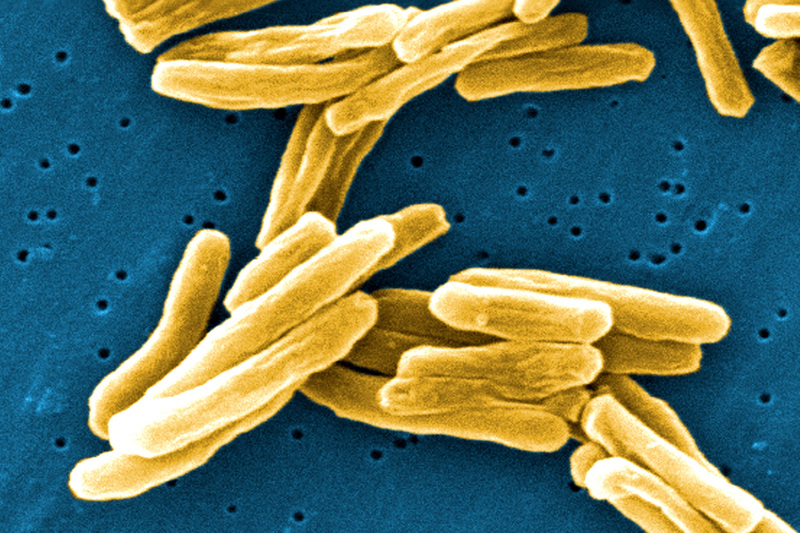
What roles do talking and breathing play in the spread of tuberculosis (TB)? How quickly does treatment prevent transmission of the infection? A University of Cape Town (UCT) research team has been awarded funding to answer these questions and in turn benefit the communities most affected by the disease.
A team of UCT scientists studying the transmission of TB has been awarded funding by the first Africa seed fund initiative from Imperial College London and the Massachusetts Institute of Technology (MIT).
The MIT-Africa-Imperial College London Seed Fund investment will go towards cooperation between the institutions via the ‘fluorTB’ consortium. The name refers simultaneously to the fluorescence imaging which is central to the project, and the need to deliver a knock-out blow (“floor”) to a disease that continues to plague South Africa and other TB-endemic regions.
The researchers will study how TB is transmitted through the air – via actions such as breathing, talking and coughing – and the role anti-TB therapy can play in limiting the disease’s spread.
“The obvious place to tackle the TB problem is to block transmission, and yet we know very little about it,” says UCT project leader, Professor Digby Warner.
“We aim to understand how the disease is transmitted through the air by bringing international expertise to our research facility based in one of the communities in Cape Town hardest hit by TB.”
“We aim to understand how the disease is transmitted through the air by bringing international expertise to our research facility based in one of the communities in Cape Town hardest hit by TB.”
A needle in 1 000 haystacks
The research is based on a simple theory: those infected with TB breathe the bacteria out into the air and infect others. But to prove this, scientists must not only capture air samples to study, but also find Mycobacterium tuberculosis (Mtb), the bacterium which causes TB, in the samples.
They do this by putting patient volunteers in a small, personalised clean room and collecting about 300 litres of their expired air, which is concentrated into just five millilitres of liquid.
“Imagine a vacuum cleaner running a cyclone of liquid, where all the particulate matter in the air is trapped in the liquid,” says Warner.
Bearing in mind that Mtb is a bacterium smaller than a human blood cell, and that expired air carries a host of other organisms and debris, Warner agrees it’s like looking for a needle in a haystack.
“Except, it’s more like looking for a needle in a thousand haystacks,” he says.
“We want to move from a research tool to a diagnostic tool. Doing that can be slow and difficult if everyone is operating at distance.”
That means the major focus of the research is to develop a method that weeds through the crowded air samples to find Mtb bacteria. The scientists must also find a way to isolate these bacteria and confirm with additional testing that they are indeed Mtb. That’s where the collaborators at MIT and Imperial can help.
Using clever chemistry, Professor Laura Kiessling’s group at MIT develops fluorescent probes which decorate the Mtb cell wall, making the bacteria light up under the microscope. This technology, in combination with the single-cell expertise of Professor Brian Robertson’s group at Imperial College, might be just the trick to speed up identification of Mtb in these “haystacks”.
On-the-ground solutions
This international collaboration is possible thanks to the seed fund, says Ryan Dinkele, a UCT PhD student and one of the microbiologists working on the project.
“It’s a fluid exchange of knowledge where we work together with our collaborators at MIT and Imperial to address the gaps in expertise that we need to find solutions,” he says.
The funding directly supports travel for scientists to and from UCT. Getting the scientists together on the ground is one of the most important ways of turning their research into solutions for patients, according to Warner.
“We want to move from a research tool to a diagnostic tool. Doing that can be slow and difficult if everyone is operating at distance,” he says.
“Does treatment stop people from transmitting within days or weeks? That might be directly measurable with our technology.”
“By having people on-site and being able to give feedback quickly, we can rapidly tailor our system to get results.”
With the bulk of the research being done at the recently opened TB Aerobiology Research Facility in the UCT Desmond Tutu HIV Foundation (DTHF) Masiphumelele site, the goal is to combine research results with targeted therapies for the community.
The lab, known by the researchers as the ‘Masi site’, is in a township where 20% of five-year-olds are infected with TB before they start school. It serves as a microcosm of the TB epidemic in Cape Town.
“Cape Town as one city has more TB cases than the United States, the United Kingdom, Germany and France combined. If you want to study how to tackle the problem, you want to do it here,” says Emeritus Professor Robin Wood, chief executive officer of the DTHF and leader of the TB Aerobiology programme.
This proximity to the disease not only gives the researchers access to patients and samples – but also boosts their passion and sense of urgency.
“Our lab is unique in the world for being built specifically to study TB transmission, but it’s also located in a place that has some of the highest rates of TB, even within Cape Town itself,” says UCT’s Dr Anastasia Koch, one of the team’s researchers.
“Cape Town as one city has more TB cases than the United States, the United Kingdom, Germany and France combined. If you want to study how to tackle the problem, you want to do it here.”
“That’s really interesting for a scientist because you’re exposed to the realities of the problem; it changes the way you think about your research and makes it more powerful and urgent.”
Making an impact
As their research starts to produce results, the team hopes their work will inform how anti-TB therapies are used. Warner says they may be able to assess the effectiveness of known therapies for blocking transmission, for example.
“We know that treatment is effective in blocking transmission, but we don’t know how quickly it does that,” he says. “Does treatment stop people from transmitting within days or weeks? That might be directly measurable with our technology.”
By answering questions like this and bringing in collaborations that strengthen its research, the Masi site has the potential to drive science that makes a difference.
“The goal is to operationalise our work while developing new technologies that we can apply in the community to control the infection rates happening outside our door,” concludes Wood.
 This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License.
Please view the republishing articles page for more information.
Newsbytes

Applications for The Pitch UCT are officially open.
17 Apr 2024 - 2 min read































