Why I choose COVID-19 vaccination based on verifiable evidence
25 January 2021 | Story Thomas Scriba. Photo Adobe Stock. Read time 7 min.
A COVID-19 vaccine is on the way, but a huge hurdle will be to convince vaccine-hesitant people to receive it. The University of Cape Town’s (UCT) Professor Thomas Scriba explains the safety profiles of the three available COVID-19 vaccines, and the benefits of receiving it.
“I’d rather take my chances with coronavirus than take a vaccine that was developed in less than a year.”
I heard this astounding sentiment quite regularly this festive season during conversations with family or friends. The various conversations around these statements suggest that thousands of people in our country, and around the globe, do not have access to reliable and accessible sources of information. As such, people are not able to make informed choices based on sound evidence.
This is not surprising given the extreme range in quality and reliability of information spread on social media and certain other media outlets. How do we tell what is real or true, what is misinformation, and what is simply fake, sensationalist news?
As someone who has spent more than 15 years studying infectious diseases and the human immune system, I have been following the scientific literature closely to keep myself informed about the latest reliable scientific evidence that has emerged. Based on verifiable and sound evidence, let us compare the risks you face after infection with the Covid-19 virus, SARS-CoV-2, with those you face if you choose vaccination against Covid-19.
I have provided a number of sources of evidence in this article – please make a point of accessing each one to verify the information and its source (which is often much more detailed than the summary that I provide). Checking sources is by far the best way to verify whether something you have read or seen is in fact reliable scientific evidence rather than an unverifiable opinion, speculation, conjecture, or even worse, misinformation.
SARS-CoV-2 infection and Covid-19 disease
Based on the current numbers of cases who test positive for SARS-CoV-2 infection and deaths attributable to Covid-19 in the 20 countries with the highest numbers of cases, the average case fatality rate is 2.7% (range 1%-8.8%). This means that out of every 1 000 people who test positive, approximately 27 die (the reported fatality rates for the 20 countries range from 10 to 88).
What is not widely talked about is that among those who survive, many more (according to some reports up to 10% or 100 out of 1 000) end up with “long Covid”. This term describes the long-lasting and very significant syndrome characterised by fatigue and serious health problems that persist after the initial Covid-19 illness.
Long Covid can affect the lungs, the cardiovascular system, the gut, the brain and the immune system, among others.
Vaccination against Covid-19: What is vaccination?
Vaccination is a way to trick our immune system into thinking that it has been infected with the virus, but without the risks of developing the disease. We do this by delivering a small part of the virus into the skin or muscle.
In the case of Covid-19, the spike protein of the SARS-CoV-2 virus is delivered, so that our immune system initiates a training programme for immune cells that will become SARS-CoV-2 spike protein specialists. Some of these Covid-19 specialist immune cells produce antibodies that find and help to eliminate the virus from the body, should it ever infect the body.
Other types of Covid-19 specialist immune cells (T cells) can identify and then kill our own cells if they have been infected and turned into SARS-CoV-2 virus manufacturing “factories”. Most importantly, these specialist immune cells can live for a very long time and they remain Covid-19 spike protein specialists so that they can do their job if a person is infected months or even many years after vaccination.
Vaccination is not a treatment (or cure) for someone who is already infected or sick. Rather, it is a strategy to train the immune system to be better equipped to deal with the infection in the future, so that infection or disease is prevented. After all, prevention is better than cure.
Evidence on Covid-19 vaccination
To make the evidence as simple to digest as possible, and to be sure that I review evidence that has already been scrutinised and “certified as reliable” by independent medical experts (referred to as scientific peer-review), I will only refer to results from the phase 3 trials that have been published in peer-reviewed scientific journals.
These publications report the results for the mRNA-1273 (Moderna), the BNT162b2 (BioNTech/Pfizer) and the ChAdOx1 nCoV-19 (AZD1222) (Oxford University/AstraZeneca) vaccines.
The reported results were collected within two to eight weeks after the first vaccination, which is early – phase 3 trials usually collect such data over several years. But reporting such early results is justified given the urgency of finding tools that can prevent Covid-19, and because the high numbers of confirmed Covid-19 cases in these trials allowed reliable comparison of individuals who received the vaccines with those who received placebo (a substance that has no effect on SARS-CoV-2 or Covid-19, such as saline solution).
Results from the longer follow-up of trial participants will be reported once available.
Can these three vaccines prevent Covid-19?
The short answer is yes; the vaccines are highly efficacious. In fact, the vaccines prevent Covid-19 to a greater degree than we expected. Here are the vaccine efficacy results in more detail:
mRNA-1273 vaccine (Moderna)
Vaccine efficacy (protection against Covid-19) was 94.1%. There were 11 Covid-19 cases among 15 210 people who received the vaccine versus 185 Covid-19 cases among 15 210 who received the placebo. Severe Covid-19 disease occurred in 30 people, all in the placebo group, and one of these individuals died. Protection against severe Covid-19 was therefore 100%.
BNT162b2 vaccine (BioNTech/Pfizer)
Vaccine efficacy was 95%. There were 8 Covid-19 cases among 21 720 people who received the vaccine versus 162 Covid-19 cases among 21 728 who received the placebo. Among 10 cases of severe Covid-19 disease, nine occurred in placebo recipients and one in a vaccinated recipient.
ChAdOx1 nCoV-19 vaccine (Oxford/AstraZeneca)
Overall vaccine efficacy was 70.4% (an average of results from the UK and Brazil). There were 30 Covid-19 cases among 5 807 people who received the vaccine versus 101 Covid-19 cases among 5829 who received the placebo. There were 10 cases with Covid-19 disease who had to be hospitalised, and all were in the placebo control group. Two of these were classified as severe Covid-19 and one of these persons died.
Are the vaccines tolerable and is their safety acceptable?
Again, the short answer is yes, as discussed below. It is important to recognise that after delivery of the spike protein during vaccination, many people experience some uncomfortable reactions at the vaccination site or more general symptoms that typically resemble a short “flu-like” illness, such as headache, fatigue, chills or muscle aches, while pain at the injection site is also quite typical. These reactions typically last one to four days.
It is tempting to think that the vaccine causes the flu and that this is dangerous. In fact, some people say that they got the flu from being vaccinated. But this is a misunderstanding of the reality that such symptoms are actually the normal signs of the immune system kicking into action.
Injection of the vaccine induces a normal inflammatory reaction so that immune cells are appropriately trained to become anti-Covid-19 specialists (remember, we are tricking the immune system into thinking it is a real infection, when it is of course not a real viral infection with risks of Covid-19 disease).
It is known from decades of experience with vaccination practices for other diseases around the globe that these early and short-lived reactions to vaccination are by far the most common adverse events. Long-term safety issues can happen, but they are unlikely and extremely rare (and certainly much, much lower than the case fatality rate of 2.7% for Covid-19 disease).
Below are more detailed summaries of the safety and tolerability results from the three trials. For more information, you can also access the publications provided in the links, which report very detailed tables and lists of events recorded in each trial.
mRNA-1273 vaccine
The results indicate that approximately 80% of those who received the vaccine experienced pain at the injection site (versus 20% of those who received the placebo) and between 55% and 75% of those who received the vaccine experienced flu-like reactions within two to four days after vaccination, including headache, fatigue, chills or muscle aches.
The most common vaccination-related adverse events (reported in at least 1% of participants) in the vaccine group were fatigue (1.5%) and headache (1.4%).
In the placebo group, 1.2% reported fatigue and 0.9% reported headache. Vaccine-related severe adverse events were higher in the vaccine group (0.5% of participants) than in the placebo group (0.2% of participants). Serious adverse events, hypersensitivity reactions and Bell's Palsy were also observed in a small proportion of trial participants, but these were not different in number between the vaccine and placebo groups.
Three deaths occurred in the placebo group and two in the vaccine group. These could not be linked in any way to the vaccine (cardiopulmonary arrest and suicide).
BNT162b2 vaccine
The findings of this trial show that approximately 80% of those who received the vaccine experienced pain at the injection site (less than 1% reported severe pain) which resolved within two days. Approximately 12% who received the placebo reported pain at the injection site.
Adverse events were generally less common in older people (above 55 years) than younger people. Fatigue and headaches were the most common systemic adverse events, reported by 60% and 52% of vaccine recipients in younger people. Fatigue and headaches in the placebo group were reported by 23% and 24% in the young.
More severe systemic events were reported in less than 2% of vaccine recipients after either dose, except for fatigue (in 3.8%) and headache (in 2.0%) after the second dose.
Fever at more than 38°C was reported after the second dose by 16% of younger and 11% of older vaccine recipients. These symptoms resolved within one to two days.
More vaccine recipients than placebo recipients reported any adverse event (27% and 12% respectively) or an adverse event that was judged to be related to vaccination (21% and 5%).
A total of 64 vaccine recipients (0.3%) and six placebo recipients (less than 0.1%) reported lymphadenopathy (swollen/sensitive lymph nodes).
Four deaths occurred in the placebo group and two in the vaccine group. These could not be linked in any way to the vaccine (e.g. arteriosclerosis, cardiac arrest, haemorrhagic stroke, myocardial infarction).
ChAdOx1 nCoV-19 (AZD1222) vaccine
The safety and tolerability of this vaccine was reported in detail in an initial paper, separate from the efficacy result. Approximately 80% of those who received the vaccine experienced tenderness or pain at the injection site which resolved within four to seven days. Many participants took paracetamol, which reduced these symptoms somewhat.
A total of 70% of vaccine recipients reported fatigue and 68% reported headaches, which were the most common systemic effects. Other side effects included muscle ache, feeling feverish, feeling unwell, as well as fever. These typically resolved within four days. Further details on serious adverse events were reported in the efficacy paper, which was published after the initial paper.
Among the 11636 who are described in the efficacy paper, serious adverse events occurred in 168 participants, 79 of whom received ChAdOx1 nCoV-19 and 89 of whom received the placebo, which was either saline or a meningococcal vaccine (MenACWY, a vaccine against a bacterium that is completely unrelated to Covid-19).
Three cases of transverse myelitis were reported. One was judged to be possibly related to vaccination and the other two (one in the ChAdOx1 nCoV-19 and the other in the placebo group) were judged unlikely to be related to vaccination by independent committees of neurological experts during trial pauses.
One participant had a fever above 40°C that resolved rapidly – allocation to vaccine or placebo was not unblinded in this case (the trial is still ongoing). Three deaths occurred in the placebo group and one in the vaccine group. These could not be linked in any way to the vaccine (road traffic accident, blunt force trauma, homicide, and fungal pneumonia).
Professor Thomas Scriba is the deputy director of immunology and laboratory director at the South African Tuberculosis Vaccine Initiative, a research unit at the University of Cape Town.
Coronavirus Disease 2019 updates
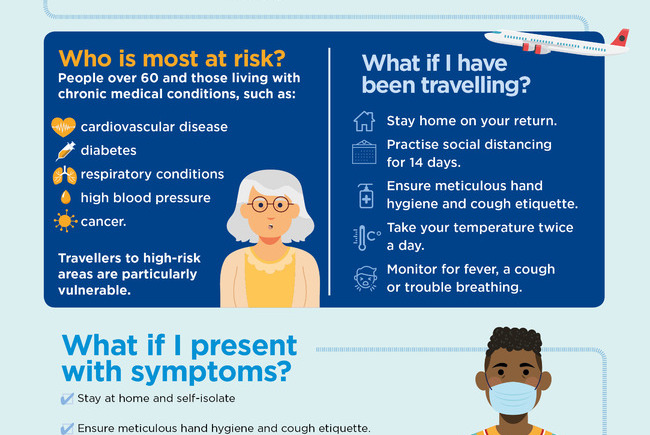
COVID-19 is a global pandemic that caused President Cyril Ramaphosa to declare a national disaster in South Africa on 15 March and implement a national lockdown from 26 March.
UCT is taking the threat of infection in our university community extremely seriously, and this page will be updated regularly with the latest COVID-19 information.
Daily updates
Campus communications
Resources
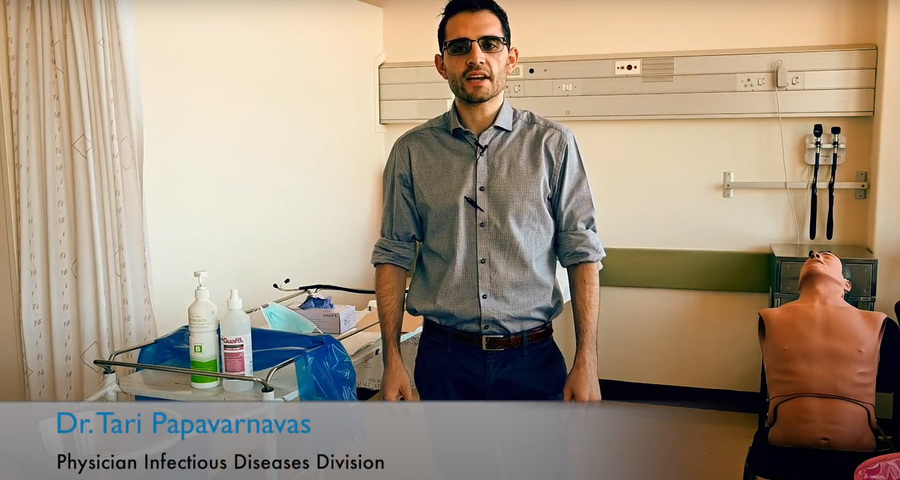
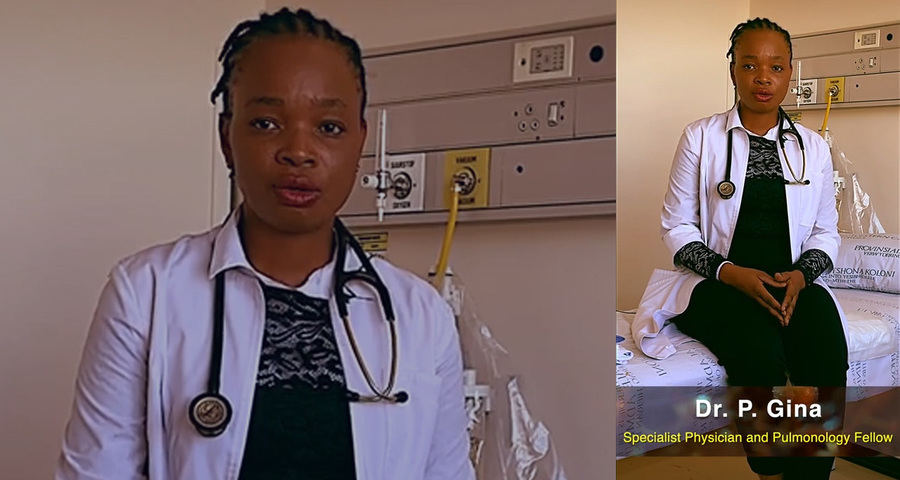
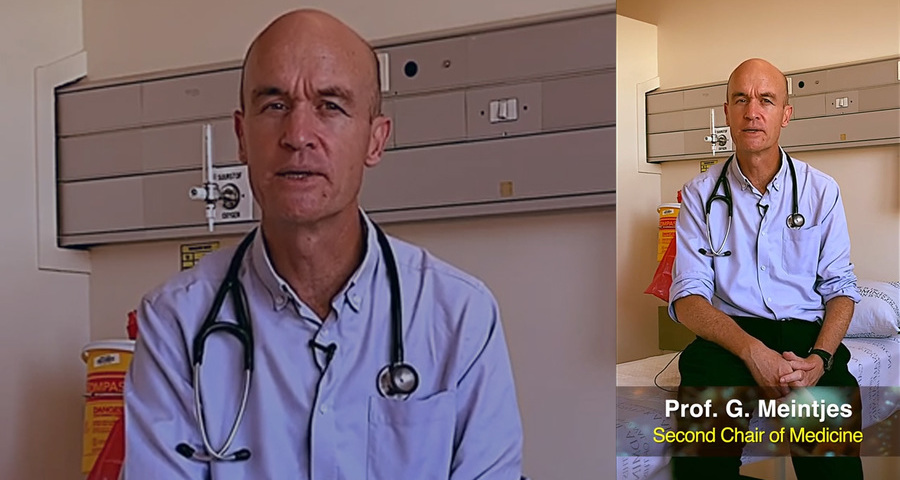
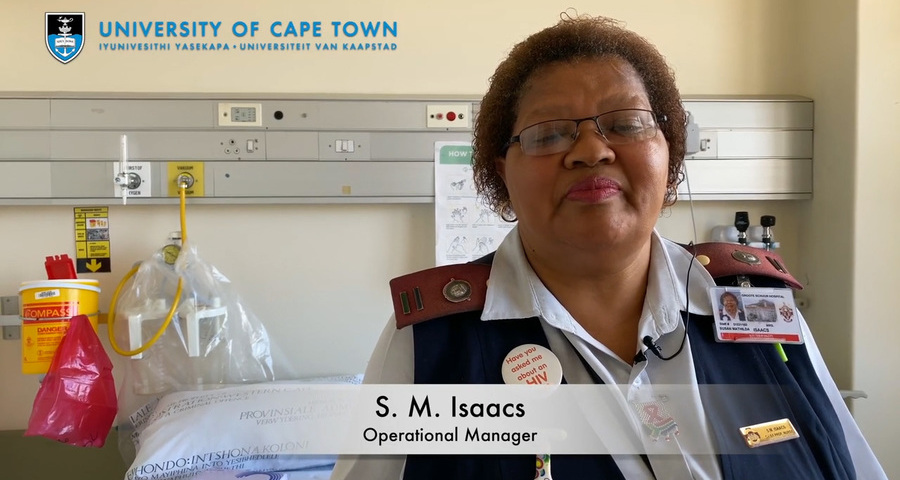
Video messages from the Department of Medicine
Getting credible, evidence-based, accessible information and recommendations relating to COVID-19
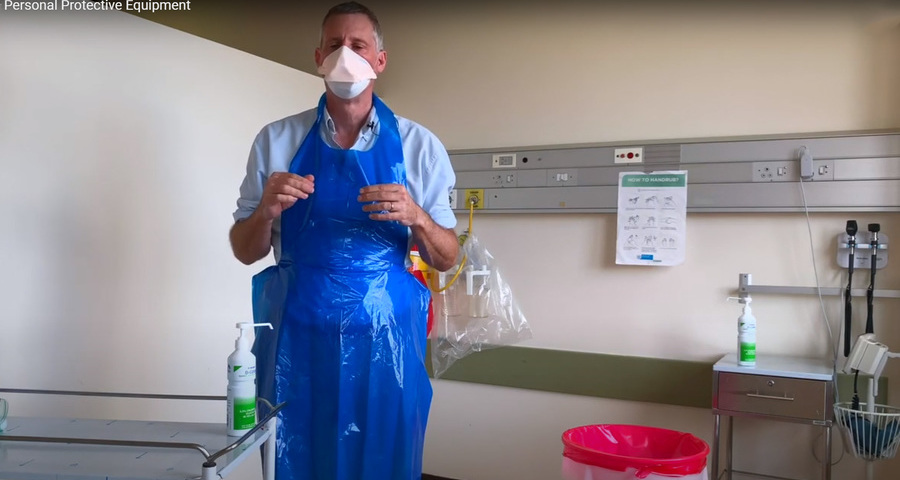
The Department of Medicine at the University of Cape Town and Groote Schuur Hospital, are producing educational video material for use on digital platforms and in multiple languages. The information contained in these videos is authenticated and endorsed by the team of experts based in the Department of Medicine. Many of the recommendations are based on current best evidence and are aligned to provincial, national and international guidelines. For more information on UCT’s Department of Medicine, please visit the website.
To watch more videos like these, visit the Department of Medicine’s YouTube channel.
Useful information from UCT
External resources
News and opinions

As the COVID-19 crisis drags on and evolves, civil society groups are responding to growing and diversifying needs – just when access to resources is becoming more insecure, writes UCT’s Prof Ralph Hamann.
03 Jul 2020 - 6 min read Republished
The Covid-19 crisis has reinforced the global consequences of fragmented, inadequate and inequitable healthcare systems and the damage caused by hesitant and poorly communicated responses.
24 Jun 2020 - >10 min read Opinion
Our scientists must not practise in isolation, but be encouraged to be creative and increase our knowledge of the needs of developing economies, write Professor Mamokgethi Phakeng, vice-chancellor of UCT, and Professor Thokozani Majozi from the University of the Witwatersrand.
09 Jun 2020 - 6 min read Republished
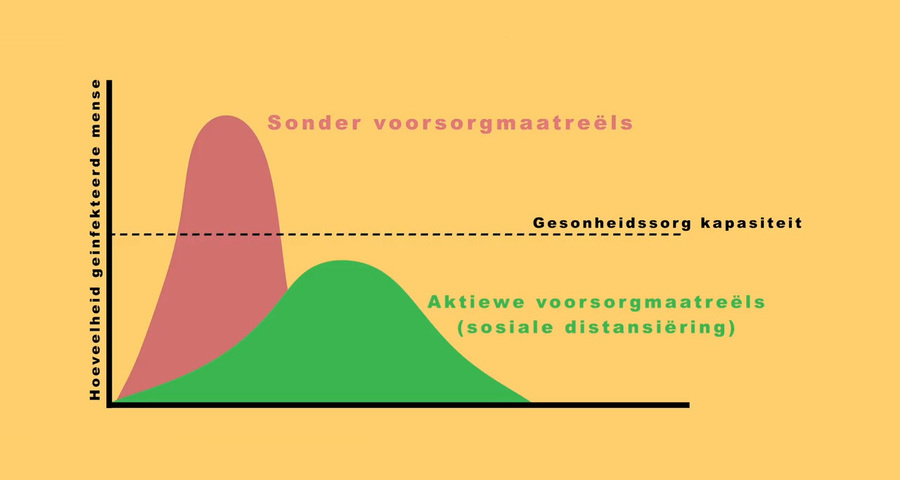
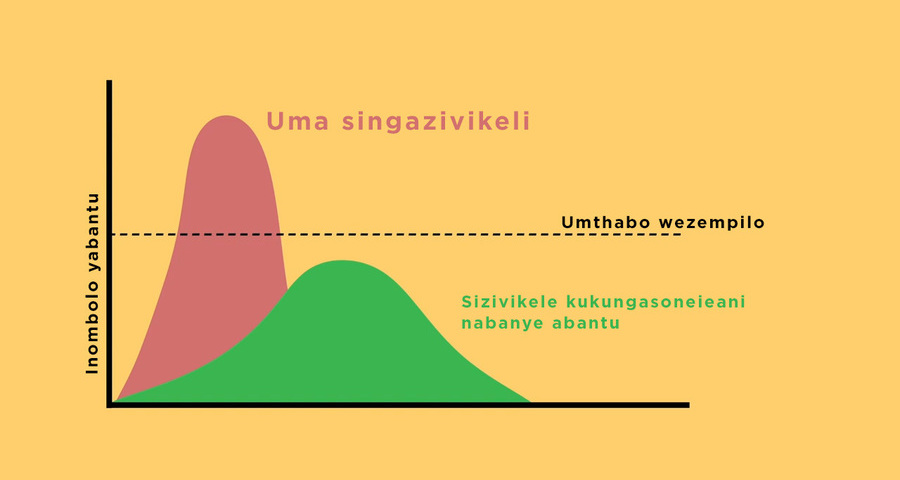
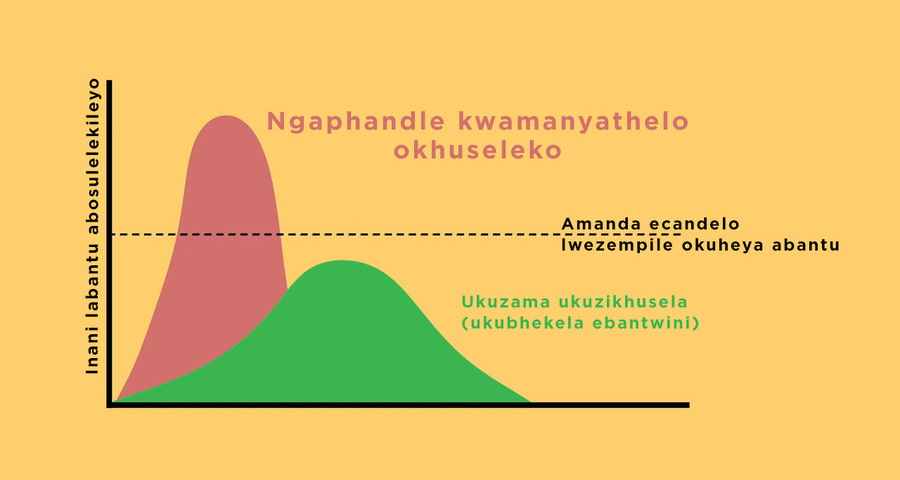
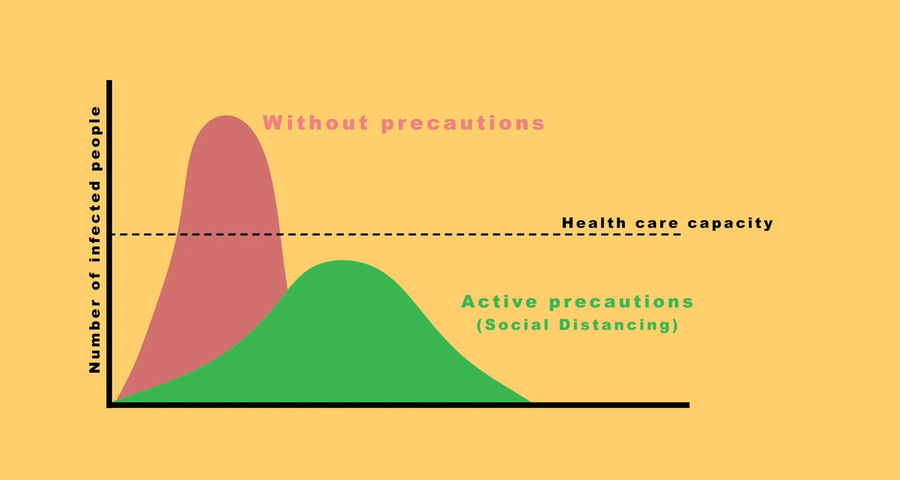
South Africa has been recognised globally for its success in flattening the curve, which came as a result of President Ramaphosa responding quickly to the crisis, writes Prof Alan Hirsch.
28 Apr 2020 - 6 min read RepublishedStatements and media releases
Media releases
Read more
Statements from Government
In an email to the UCT community, Vice-Chancellor Professor Mamokgethi Phakeng said:
“COVID-19, caused by the virus SARS-CoV-2, is a rapidly changing epidemic. [...] Information [...] will be updated as and when new information becomes available.”
We are continuing to monitor the situation and we will be updating the UCT community regularly – as and when there are further updates. If you are concerned or need more information, students can contact the Student Wellness Service on 021 650 5620 or 021 650 1271 (after hours), while staff can contact 021 650 5685.